

3 Workforce Strategy Imperatives

Health care executives have no shortage of core issues to solve for today. Managing population health, achieving health equity and transforming care delivery during a pandemic are just a few of the top priorities. Overarching all of these issues is the increasingly pressing concern of a workforce shortage.
A clinical workforce strategy has become paramount as the field seeks to address the ongoing shortages of physicians, nurses and other mission-critical positions. The recently released AHA 2022 Talent Scan from the AHA Workforce Strategy team provides a road map for addressing: resilience, flexibility, capacity and strategy.
Key to these efforts will be rethinking clinician education and training for everyone from students to leaders. The pandemic continues to interrupt and disrupt the education of clinicians in training. At the same time, it fundamentally shifted how care likely will be delivered in the future, which has myriad implications for training, retraining and upskilling current and future clinicians.
A Prescription for Pandemic Interruptus
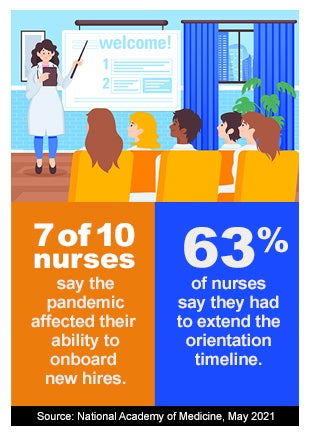
Health care organizations will need to revamp and ramp up training and onboarding for new clinicians. Seven of 10 nurses said the pandemic has affected their ability to onboard new hires and 63% said they had to extend the orientation timeline, according to a National Academy of Medicine report from May.
 Many recent graduates also had gaps in their clinical experience when the pandemic forced profession schools to suspend or limit in-person clinical instruction. Instead, training often leaned heavily on virtual/simulation or nonbedside areas like quality improvement.
Many recent graduates also had gaps in their clinical experience when the pandemic forced profession schools to suspend or limit in-person clinical instruction. Instead, training often leaned heavily on virtual/simulation or nonbedside areas like quality improvement.
Likewise, the exponential rise in virtual visits as hospitals and health systems scaled their telehealth offerings has surfaced physician training needs. Eighty-five percent of physicians believe training to improve skills like conveying empathy during virtual visits is essential but lacking in their practices, according to a 2020 Deloitte survey.
An Urgency for Critical-Thinking Skills
The sheer quantity of medical literature and fast pace of medical advances means that tomorrow’s physicians will need to cultivate the ability to assimilate new knowledge through critical-thinking skills, rather than rely on their residency training or personal experience. Physician training and education also must adapt to the learning styles of millennials by incorporating more group-based projects, informal teaching sessions (rather than traditional lectures) and an increased emphasis on why new information is relevant.
New Flexibility and Needs Demand New Skills
During the pandemic, more than 60% of nurses floated across units, acuity levels and settings — nearly twice the previous rate. About one-third are interested in continuing to do so, indicating the value of cross-training. One-third of front-line nurses also expressed concern that they do not have the skills they need for future success in a role that is evolving quickly. They expect their employers to clarify clinical guidelines for new delivery care models and technology requirements, as well as to provide access to the necessary training.
3 Ways to Address Workforce Needs
Boost flexibility with multiple staffing models
Optimize nursing resources by using a variety of staffing models, including team-based staffing (where one RN supervises a team of licensed practical nurses, aides and technicians); tiered staffing to augment experienced intensive care unit staff by incorporating non-ICU staff of all disciplines; and functional care delivery in which a nurse manager coordinates care by delegating tasks through a hierarchical structure.
Build professional as well as clinical skills
Interpersonal communication, delegation, evidence-based practice, leadership and other professional skills often challenge new clinicians more than clinical proficiency. Explore innovative ways to supplement teaching these skills, including engaging and immersive experiences through videoconferencing and virtual education.
Support diverse learning styles
As education and training increasingly become hybrids of virtual and in-person opportunities, strategically plan to ensure consistency across your organization. No matter which platform is used, ensure that your curriculum meets the needs of clinicians with diverse learning styles. The opportunity for open dialogue between new health care professionals and their support teams is also a crucial component, enabling immediate feedback, clarification of questions or issues, and follow-up on progress or concerns.



