Issue Brief: Patients and Providers Faced with Increasing Delays in Timely Discharges
December 2022
The Issue
Patients requiring additional care after a hospitalization — such as skilled nursing, behavioral health or therapy-at-home — face growing delays in accessing that care. Delays in discharges as patients move through the continuum of care can cause harm to patients’ health outcomes and can impact their quality of life by slowing their recovery. These delays also put incredible strain on hospitals and health systems as they must bear the costs of caring for patients during those excess days without appropriate reimbursement, and they also add burden on an already thin workforce. This strain comes atop the ongoing toll of the COVID-19 pandemic and recent economic trends that have exacerbated hospitals’ financial challenges, including significant increases in the costs of providing care to patients.
It is clear these delays are occurring concurrently with severe health care workforce shortages among both clinical and non-clinical workers. These shortages have been challenging for acute care hospitals as well as post-acute care and other providers receiving patient transfers from acute care hospitals, such as psychiatric hospitals. As a result, post-acute care and other providers have been unable to accept new patients, creating patient bottlenecks at acute care hospitals. Rehabilitation and long-term care hospitals also report similar patient bottlenecks with difficulties discharging their patients to other post-acute care providers, such as skilled nursing facilities.
Patients Waiting for Discharge to Post-acute Care Providers Are Staying Longer in the Hospital
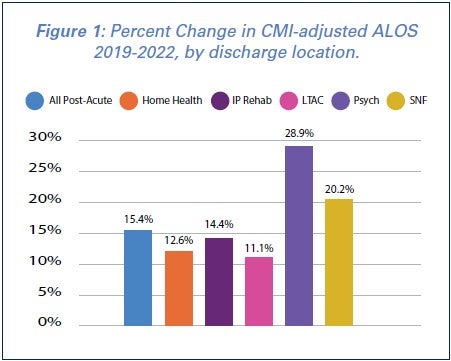 Data from Strata Decision Technology, a health care technology and consulting firm, show that the average length-of-stay (ALOS) in hospitals has increased 19.2% across the board for patients in 2022 as compared to 2019 levels. The increase is more pronounced for patients being discharged to post-acute care providers — with an increase in ALOS of nearly 24% from 2019 to 2022. This remains true even after accounting for patients being sicker and requiring more complex and intensive care now as compared to pre-pandemic levels, as measured by the case mix index (CMI).
Data from Strata Decision Technology, a health care technology and consulting firm, show that the average length-of-stay (ALOS) in hospitals has increased 19.2% across the board for patients in 2022 as compared to 2019 levels. The increase is more pronounced for patients being discharged to post-acute care providers — with an increase in ALOS of nearly 24% from 2019 to 2022. This remains true even after accounting for patients being sicker and requiring more complex and intensive care now as compared to pre-pandemic levels, as measured by the case mix index (CMI).
Additionally, CMI-adjusted ALOS has increased for patients being discharged from acute care hospitals to post-acute care providers, with a 12.6% increase for patients being discharged to home health agencies and a 20.2% increase for patients being discharged to skilled-nursing facilities (SNFs). Similarly, patients being discharged from acute care hospitals to other hospital settings have also seen increases, with a 28.9% increase for discharges to psychiatric hospitals. (See Figure 1 above).
Support Needed for Hospitals
These costs are further straining hospitals across the country that are already dealing with a range of financial pressures from historic levels of inflation to skyrocketing costs, as well as their own workforce challenges. Data from the health care consulting firm Kaufman Hall found that hospitals’ expenses are projected to increase by $135 billion in 2022 alone, with 68% of hospitals projected to end the year operating at a financial loss.
To help mitigate the costs of caring for patients for these excess days in the hospital and to ensure that patients are getting the most appropriate care possible, the AHA is asking Congress to establish a temporary per diem Medicare payment targeted to hospitals, including acute, long-term care, rehabilitation, and psychiatric, to ease capacity issues. This per diem payment would be made for cases identified and assigned with a specific discharge code that fall under such type of long stays where the patient is documented to be ready for discharge but is unable to be discharged appropriately. The solution could be modeled after an existing per diem Medicare payment mechanism and be temporary with a cap on payments.
It is critically important to ensure that hospitals and health systems remain financially stable, so that they can continue to provide high quality care to patients and communities throughout the country.