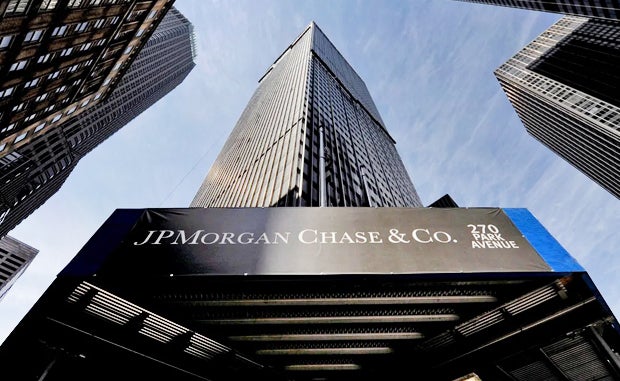
Three Takeaways from the J.P. Morgan Health Care Conference
In just about any other setting, it might be considered bad form for a host to upstage its guests. Not so at last week’s J.P. Morgan Health Care Conference. The investment banking giant’s health care arm Morgan Health made some of the biggest news amid developments from health care startups, providers, tech developers, biotech and pharma firms.
 Can Reshaped Accountable Care Lower Costs?
Can Reshaped Accountable Care Lower Costs?
When it launched in May, Morgan Health made clear its goal to disrupt primary care by reshaping employer-sponsored health plans to drive down costs. What hasn’t been clear is how it plans to do this. At the event, Morgan Health revealed two partners with whom it will collaborate to help achieve its vision.
In a new partnership with Kaiser Permanente, about 8,000 JPMorgan Chase employees in California this month will be able to access care through the health system. This integrated structure will allow data to be gathered not just from claims but also from electronic health records to provide a more complete picture of each patient’s health.
These data also will help both organizations collect and report health metrics for JPMorgan employees and to improve health equity. The organizations plan to issue performance guarantees tied to health equity based on certain quality measures for JPMorgan employees beginning in 2023.
In addition, Morgan Health will test its primary care model in a pilot where patients can receive care digitally while also having some flexibility to choose specialists outside their immediate health system. The pilot also will test Seattle-based Vera Whole Health’s model, in which Morgan Health has invested $50 million. Vera Whole Health runs a network of primary care centers across 10 states and has a relationship with Central Ohio Primary Care. Vera Whole Health also bought Castlight, a care navigation company that helps guide employees to the higher-quality but lower-cost providers.
About half of Morgan Health’s Columbus, Ohio-area employees now get their care through Central Ohio Primary Care, one of the nation’s largest physician-owned primary care practices.
Pulling all these efforts together will take time, Morgan Health CEO Dan Mendelson said, adding that the company will focus on five-year outcomes as opposed to what can be accomplished in the next year.
 Stay Focused on Growth Opportunities
Stay Focused on Growth Opportunities
Amid the ongoing challenges of the pandemic, some provider organizations continue to advance their growth strategies. Intermountain Healthcare leaders noted that their ongoing shift away from fee-for-service care and toward geographic expansion is accelerating.
Intermountain’s acquisitions of HealthCare Partners Nevada, Saltzer Health and air transport company Classic Air Medical have helped the health system push into new markets. The HealthCare Partners acquisition showed Intermountain how to responsibly move a greater share of its business into value-based care arrangements, Bert Zimmerli, chief financial officer, said.
Mass General Brigham leaders, meanwhile, are focused on making growth investments in virtual care, digital tools and hospital at home while also investing some resources into cutting-edge areas like gene and cell therapies. It hopes that these latter investments one day can generate commercial revenues to fund the organization’s mission.
 COVID-19 Isn't Over by a Long Shot
COVID-19 Isn't Over by a Long Shot
COVID-19 continues to exact a heavy price on hospitals and health systems that presented at the conference. Even though Universal Health Services’ patients with omicron are not as sick as those with previous variants, they are staying in hospitals longer, said Steve Filton, CFO.
The situation is adding to workforce expenses as the for-profit health system with 27 acute care hospitals and 335 inpatient behavioral health hospitals has had to hire more contract labor to handle the influx of patients with COVID-19. Exacerbating the situation is the fact that more caregivers are becoming infected with the virus.
Illustrating just how far the pandemic is from being over, Quest Diagnostics Chairman Steve Rusckowski said COVID-19 testing has become a permanent part of his labs’ menu of tests. Patients and physicians want to test for various respiratory illnesses after detecting symptoms. He added that antibody tests that try to identify whether a patient has previously had COVID-19 will play a larger role in how clinicians manage immunity in the future.



