Confronting Coronavirus: Assessing COVID-19's Future Impact
Experts Analyze Health Care’s Near- and Long-Term Operations
Leaders Expect Bumpy Road Ahead
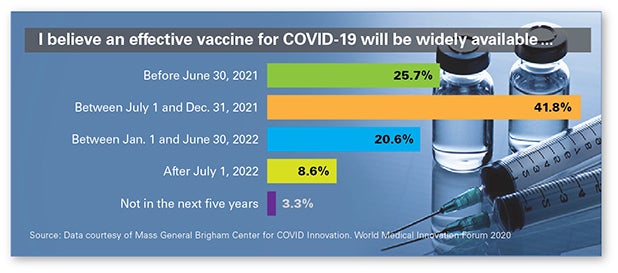
The U.S. economy has started to reopen as the impact of COVID-19 gradually subsides, but four of five senior health care leaders surveyed recently expect a significant spike in cases in their regions by fall and more than 74% do not believe an effective vaccine will be widely available until after July 1, 2021. However, nearly 61% believe an effective testing system will be offered by multiple providers in their areas between July and the end of this year.
These were just a few of the findings from a survey of more than 1,200 senior global health care leaders who took part in the World Medical Innovation Forum, hosted by Mass General Brigham. Survey participants — CEOs, CMOs, physicians, researchers and others — also expect COVID-19’s impact on society to be deep and long-lasting. Fully half of respondents expect society to be materially diminished (e.g., structural unemployment, reduced optimism), while 39% expect it to improve with a greater focus on wellness and a sense of community.
Respondents are also convinced that over the next five years, both private and government-funded investment in infectious disease research and monitoring will increase. And, more than four out of five respondents expect funding to increase by 10% or more in these areas.
9 Ways Virus May Turn U.S. Health Care on Its Head
STAT recently surveyed a host of prominent health policy experts — top health advisers to both Republican and Democratic presidents, lawmakers, executives, physicians and top lobbyists — who forecast a new status quo that they believe will upend what American health care looks like for decades. Among their predictions: The pandemic could help bring about an end to the American tradition of tying health insurance to employment status. It could prompt a reckoning about why African Americans and other historically marginalized populations have long suffered so disproportionately — not just from COVID-19, but from nearly every common health condition. And it could represent the beginning of the end for the very concept of nursing homes and assisted-living facilities.
On the Road to Financial Recovery
COVID-19’s Impact on Credit Ratings
As hospitals and health systems continue to respond to the pandemic, they’re dealing with unprecedented demand on their resources and capacity. This has had a significant impact on their financial situations. A new resource, “The Impact of COVID-19 on Hospital Credit Ratings,” provides highlights from a recently convened members-only Town Hall with the three major credit rating agencies — Fitch, Moody’s and S&P. The report encapsulates perspectives from each agency on hospital and health system credit ratings, consideration for accessing capital, meeting bond covenants and more.
How Health Care Can Recover Faster Financially
In a Harvard Business Review study of 4,900 companies across several recessions, the authors found that the optimal strategy was a combination of balanced cuts (play defense) with selective investments (play offense) before the shock or crisis was over. This approach leads to a 76% higher chance of pulling ahead of the competition when times get better than simply cost-cutting alone.
Virtual Care Performance during Crisis Reshaping Future
How Has COVID-19 Affected Perceptions about Telehealth Services?
With a surge of telehealth visits in the midst of a global pandemic, SYKES, a customer engagement services provider, surveyed 2,000 adults nationwide to understand how they perceive virtual health care and their experiences with telehealth. The survey showed that patients generally viewed telemedicine favorably, but there was room for improvement in adoption and quality.
Two-thirds of respondents said that COVID-19 had increased their willingness to try telehealth in the future. The convenience of a telehealth visit appealed to patients: quicker access to care (38%); avoiding overcrowding of clinic and hospital waiting rooms (22%); no need for transportation (16%); and greater access to care in remote areas (16%). Skepticism around quality of care and preference for a face-to-face with their caregiver were key reasons for those who would not consider a future telehealth visit. An AHA resource “Telehealth: Virtual Care Best Practices for COVID-19” provides information on how hospitals and health systems are leveraging telehealth and online tools.
Banner Health Opens Virtual Waiting Rooms
Phoenix-based Banner Health is launching virtual waiting rooms across its Banner Medical Group practices. That encompasses 300 clinics across Arizona, California, Colorado, Nebraska, Nevada and Wyoming. Working with technology company LifeLink, Banner Health is using mobile chatbots to help patients check in remotely for medical appointments before they step into the clinic. The virtual waiting room is being used for telehealth visits and in-person appointments to support COVID-19 social distancing guidelines.
AHA Tools Improve Front-Line Communications
Overcoming Communication Challenges
The pandemic has created many communication challenges for front-line staff, both in optimizing teamwork and in talking with patients and family members. The AHA has created tools to help clinical and nonclinical personnel in these stressful times:
- “Proactive Conversations that Support Providers and Patients” addresses how to effectively communicate with patients at the time of registration, admission or in the event of care escalation.
- “Proactive Care Planning and Respecting the Patient and Family Choice” provides clinical teams with a clear plan detailing what matters most to each patient and honors the preferences of the patient and family.
- “Addressing Emotions on the Front Lines” identifies techniques for front-line providers to use when patients experience increased emotion, worry or frustration. Using empathy, active listening and transparency enable hospital staff to provide support to patients and their families, build trusting relationships and defuse conflicts even in times of crisis.
“TeamSTEPPS Video Training for the COVID-19 Crisis” was developed for high-functioning teams and provides tools to optimize teamwork and communication during the pandemic. Each of six short videos focuses on one TeamSTEPPS tool and how it can be used in COVID-19 scenarios, including task assistance, closed-loop communication and briefs/debriefs and huddles.
Business Community Steps Up to Help Providers Respond
Contactless Visits of the Future
Rebuilding patient confidence will be key to bringing patients back to health care facilities. With patients delaying care out of concern for their health, providers must employ a multipronged approach that carefully considers virtual vs. in-person visits, enables a contactless experience, optimizes space to enable social distancing and redesigns workflows. Officials from the AVIA Innovator Network will discuss these issues in a free webinar May 27 at noon CT. Content will focus on how to safely resume ambulatory visits, redesign the experience for the future and recover lost revenue.
Empathetic Communication Support During COVID-19
During the pandemic, the mental state of health care workers is taking center stage as clinicians face delivering difficult news to patients and their families about what is happening, what to expect and how to prepare. RLDatix offers a free on-demand training webinar demonstrating how the lines of communication for patients and care teams can mitigate the negative consequences of this crisis and support health care workers as they seek emotional first aid, a sense of well-being and improved morale. Learn more and access the webinar.
The AHA COVID-19 website has the latest tools and resources to help hospitals and health systems respond to the pandemic.
We want to hear from you! Please send your feedback to Bob Kehoe at rkehoe@aha.org.