New Analysis Shows Hospitals Improving Performance on Key Patient Safety Measures Surpassing Pre-pandemic Levels

A new report from the American Hospital Association using data analyzed by Vizient finds that hospital performance on key patient safety and quality measures is better in the first quarter of 2024 than it was before the COVID-19 pandemic, and that hospitals made these improvements while caring for patients with more significant health care needs.
In the years prior to the COVID-19 pandemic, hospitals across the country achieved success in improving key markers that measure patient safety, including reducing infections, expediting the diagnosis and provision of lifesaving treatments for heart attack and stroke, and preventing unnecessary readmissions. Unsurprisingly, the COVID-19 pandemic disrupted that progress. However, new data analyses show not only a rebound but an improvement on pre-pandemic performance in patient safety.
While hospitals are proud of the progress they continue to make, they also recognize that there is still work to be done. Hospitals’ commitment to improving patient outcomes, advancing equity of care, and enriching the patient experience continues to drive efforts. The data in this report underscore the resilience and unwavering commitment of hospitals and health systems — and the millions of hospital team members across the country — to delivering better care and outcomes to the patients and communities they serve.
About the Data
To measure this progress, AHA partnered with Vizient, Inc., an independent, third-party, multi-faceted organization that supports hospitals and health systems in their efforts to deliver high quality care as efficiently as possible.
Key Takeaways
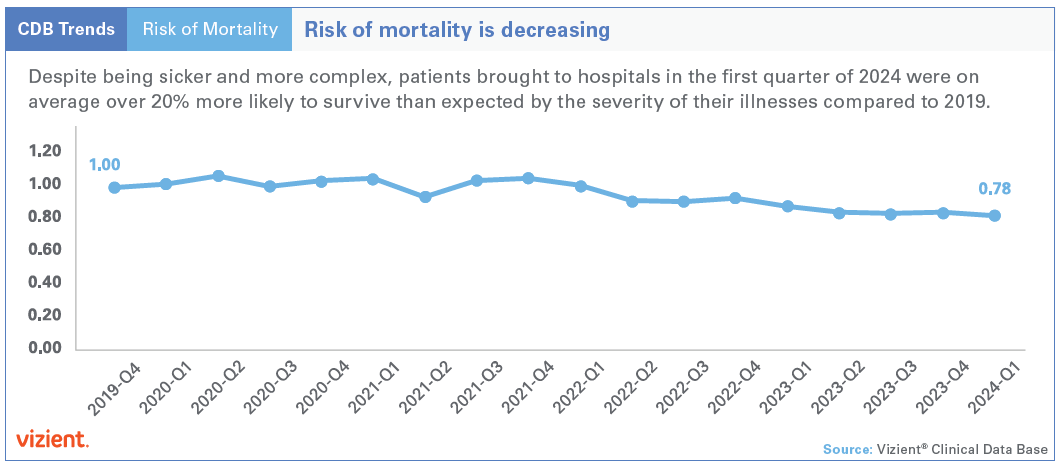
- Despite being sicker and more complex, hospitalized patients in the first quarter of 2024 were on average over 20% more likely to survive than expected given the severity of their illnesses compared to the fourth quarter of 2019.
- Based on Vizient’s analysis, the AHA using national hospitalization data projects that while caring for sicker patients, hospitals’ efforts to improve safety led to 200,000 Americans hospitalized between April 2023 and March 2024 surviving episodes of care they wouldn’t have in 2019.
- Hospitals cared for more patients overall in the first quarter of 2024 than in the last quarter of 2019, including providing care to a sicker, more complex patient population.
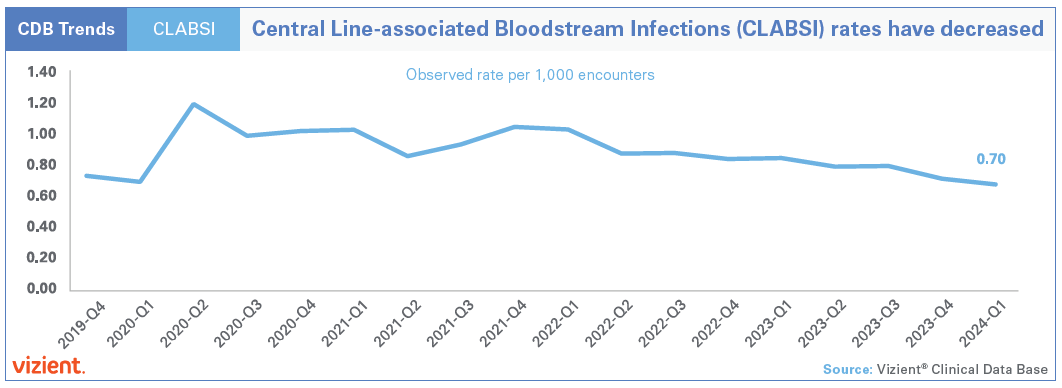
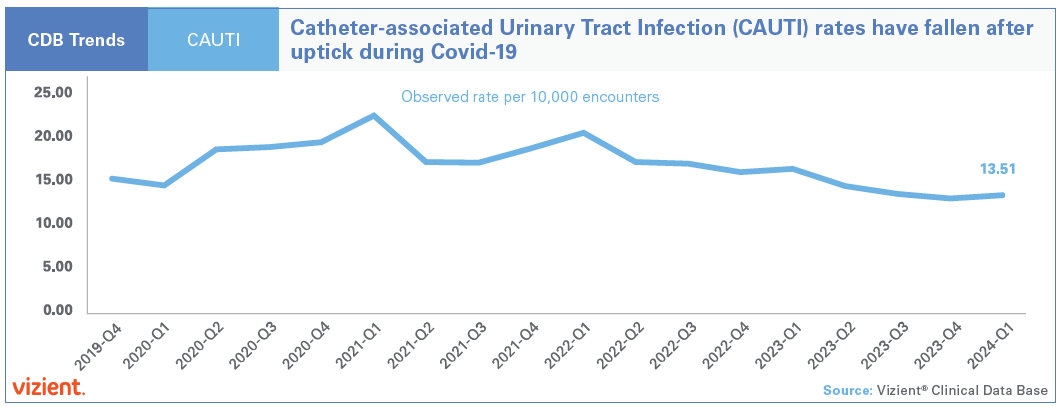
- Hospitals’ central line-associated bloodstream infections (CLABSI) and catheter-associated urinary tract infections (CAUTI) in the first quarter of 2024 were at rates lower than those recorded in the fourth quarter of 2019.
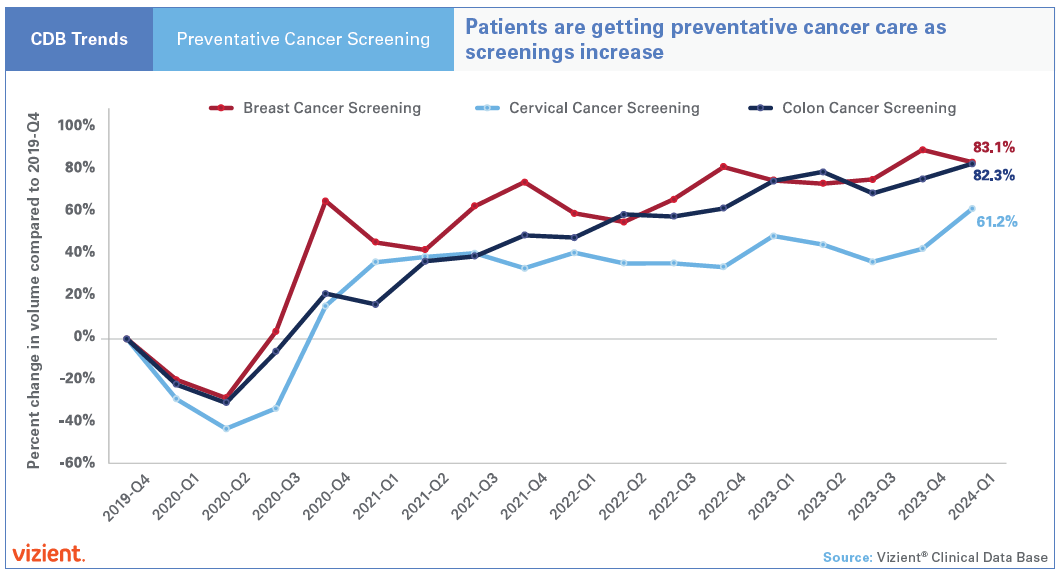
- Not only did multiple key preventive health screenings rapidly rebound to pre-pandemic levels, but ongoing improvement has led to a 60%-to-80% increase in breast, colon and cervical cancer screenings in the first quarter of 2024 compared to the fourth quarter 2019.
This analysis was entirely performed by Vizient team members and was powered by data from hospitals that routinely report clinical information to Vizient’s Clinical Data Base (CDB). The database contains information on more than 1,300 hospitals, submitted within 30 days of the end of each quarter. This provides real-time feedback to the participating hospitals and allows them to benchmark their performance against that of other general acute care hospitals. Data from the Vizient® Clinical Data Base was used with permission of Vizient, Inc. All rights reserved.
Vizient receives data on more than 10 million inpatients and 180 million outpatients annually. To analyze the trends from pre-pandemic through first quarter of 2024, Vizient identified a cohort of 715 general, acute care hospitals for which it had a complete 18 quarters of data from fourth quarter 2019 through first quarter 2024. These hospitals represent the wide spectrum of hospitals across 49 states and the District of Columbia, including the ranges outlined below.
| Comprehensive Academic Medical Center | 16% |
| Large, Specialized Complex Care Medical Center | 21% |
| Complex Care Medical Center | 23% |
| Community Hospital | 41% |
*See definition in appendix.
Hospitals and health systems have long been transparent in sharing progress on key performance measures with the public, including through Medicare’s Care Compare website. While Care Compare and other hospital rating programs can provide patients with useful information, that data can be up to three years old by the time they are public.
One of the goals of AHA’s partnership with Vizient on this project was to help provide patients, policymakers and the public with a more timely, accurate look at how hospitals are performing now instead of relying on older and sometimes outdated data. These new data show an encouraging acceleration of progress on key outcomes.
Hospitals Are Serving More Patients
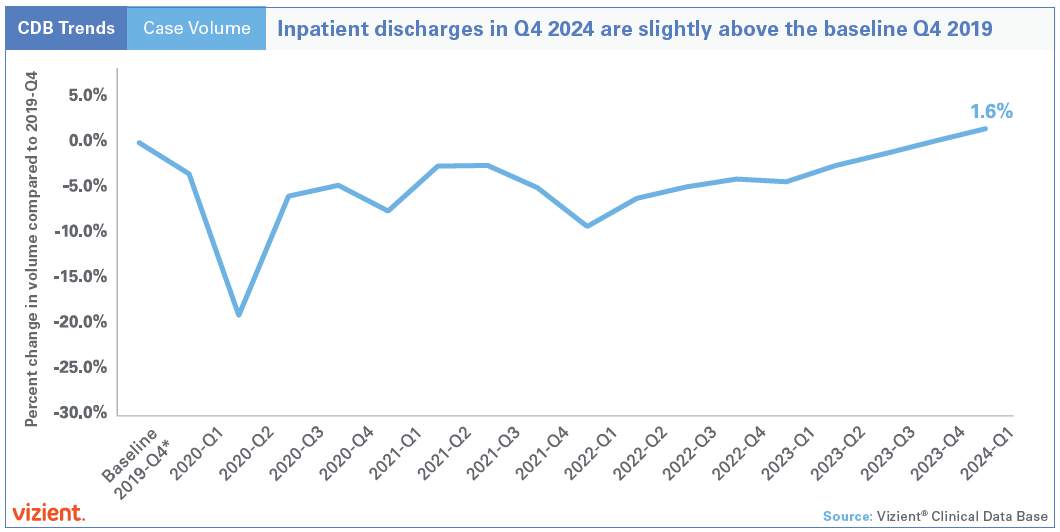
As the nation navigated the COVID-19 pandemic in 2020, hospital admissions decreased substantially to free up beds, and scheduled surgeries were postponed so hospitals could preserve supplies, personal protective equipment and other resources.
When restrictions began to ease, patients began to return to the hospital for care. Hospitals had to balance this volume rebound at the same time as periodic — and often substantial — surges in COVID-19 hospitalizations.
Once COVID-19-related-hospitalizations slowed, hospitals expected a related decrease in patients. While discharges did decrease since the most challenging months of the pandemic, they are still nearly 2% higher than pre-pandemic. Hospitals served, and continue to serve, all patients who need care.
Hospitals Are Caring for Sicker, More Complex Patients Today than Prior to the Pandemic
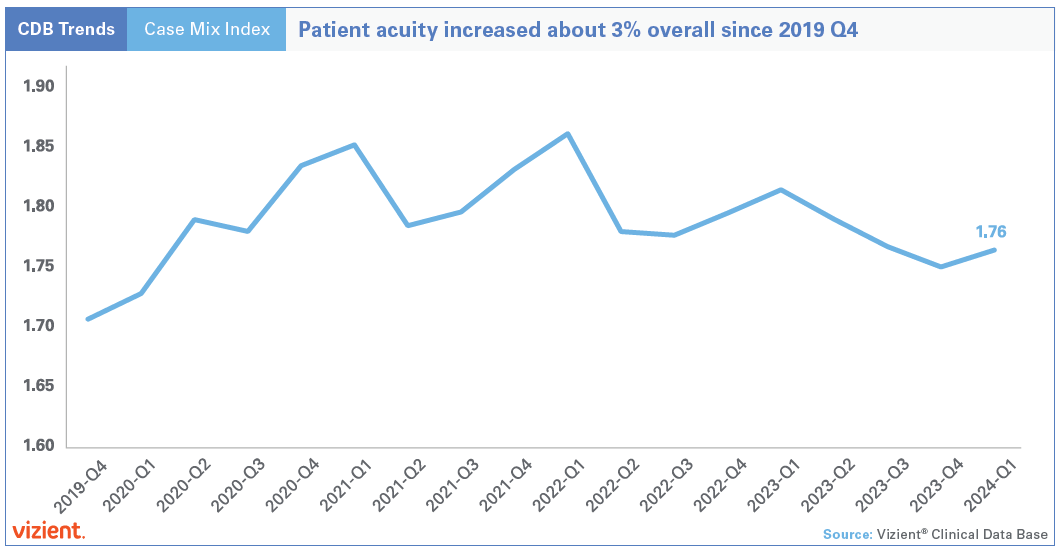
Patient acuity refers to the severity and complexity of a patient’s medical condition. Case mix index provides a nationally standardized way to estimate patient acuity by capturing the intensity of resources used to care for patients. Higher patient acuity means that patients are more critically ill or have more complex health issues.
The Vizient data finds that compared to 2019, patient acuity has increased 3%, indicating that hospitals are now serving patients with a wide spectrum of more severe conditions or more complicated illnesses.
In short, at the same time hospitals are seeing more patients, they also are seeing higher acuity patients who require more complex care. Despite these trends, the analysis shows that key patient outcomes have improved.
Risk of Mortality Is Decreasing
Risk-adjusted mortality measurements are one way to assess how well hospitals are delivering safe and timely care. For many years, hospitals and public health officials have determined the success of efforts to reduce mortality by looking at the expected mortality rate of a patient population versus the actual mortality rate. Comparing actual mortality to expected mortality involves evaluating the actual number of deaths (observed) in hospitals against the number of deaths predicted based on models like those that the Centers for Medicare & Medicaid Services uses in its Value-based Purchasing program that account for multiple contributing factors (expected). When observed mortality is consistently lower than expected — e.g., when risk of mortality is less than 1 — it indicates that more people are surviving conditions that otherwise would be expected to be fatal, suggesting ongoing continuous improvement in patient care and treatment.
The analysis, which uses Vizient’s risk-adjustment methodology, shows that since 2022, hospital mortality rates have been better than expected and that the difference between expected and observed continues to grow. In the first quarter of 2024, risk of mortality in the Vizient analysis reached 0.78 or nearly 22% lower than its baseline of 1.0 in 2019. Based on Vizient’s analysis, the AHA using national hospitalization data projects that while caring for sicker patients, hospitals’ efforts to improve safety led to 200,000 Americans hospitalized between April 2023 and March 2024 surviving episodes of care they wouldn’t have in 2019.
Infections Are Decreasing
During the pandemic, hospitals experienced an increase in certain hospital-acquired infections, partly due to the heightened use of high-risk lifesaving invasive procedures. CLABSIs and CAUTIs saw increases during the pandemic.
However, as health care systems adapted to the challenges posed by the COVID-19 pandemic and implemented effective safety practices, these infection rates have since decreased.
Currently, both CLABSI and CAUTI rates are at levels lower than those recorded in 2019. The analysis suggests improvements in infection prevention measures as hospitals continue to optimize their practices and respond to evolving patient needs.
Patients Are Getting Preventive Care as Cancer Screenings Increase
Early detection is crucial for improving health outcomes in patients fighting cancer. Timely identification leads to more effective treatments and higher survival rates, and we know that during the peak of the pandemic access to certain aspects of preventive care suffered.
Since 2019, there has been a notable increase in screenings for breast, colon and cervical cancers in two phases.
First, by the winter of 2020 these screening rates collectively exceeded the levels seen immediately before the pandemic, which highlights the dramatic efforts by hospitals, health systems and other caregivers to expand access. Since then, ongoing expansions to screening guidelines and options for screening have expanded the recommended age ranges and risk factors for testing, resulting in more individuals qualifying for testing earlier. There also have been advancements in screening methods, particularly for colon cancer — such as the adoption of less invasive testing options — that encourage more patients to choose to be screened.
Increasing efforts to promote and facilitate screenings has further boosted participation rates, emphasizing the importance of early detection and its role in improving cancer care and outcomes.
Continuous Focus on Advancing Quality and Patient Safety
All hospitals and health systems strive to deliver safe, high-quality care to every patient they serve. The AHA’s Patient Safety Initiative, which was launched in 2023, is a collaborative, data-driven effort that helps hospitals and health systems work together to reinforce and accelerate patient safety efforts. The initiative provides hospitals with tools and data to advance patient safety, offers a platform for sharing their stories of improvement with peers, and highlights examples of applicable innovation that support, spread and sustain safety improvement. For more information, visit AHA’s Patient Safety Initiative webpage.
Appendix: *Vizient Cohort Definitions
Comprehensive Academic Medical Center Criteria:
- At least 25 Solid Organ Transplants annually
- At least 600 Trauma Service line cases OR 1500 acute transfers in annually
- At least 125 combined cases Neurosurgery and Cardiothoracic Surgery annually
Large, Specialized Complex Care Medical Center Criteria:
- At least 25 solid organ transplants and 75 combined cardiothoracic and neurosurgery cases
- Or 600 trauma and 75 combined cardiothoracic and neurosurgery cases
- Or 1500 acute transfers in from another acute facility and 75 combined cardiothoracic and neurosurgery cases
Complex Care Medical Center Criteria:
- Not in the Comprehensive Academic Medical Center category or Large Specialized Complex Care category
- At least 25 combined cases Neurosurgery and Cardiothoracic Surgery annually
Community Hospital Criteria:
- Not in the previous described categories, excluding Critical Access & Specialty Hospitals
- Hospitals not included in the category criteria are critical access hospitals and specialty hospitals (cancer hospitals, children’s hospitals, other specialty hospitals).