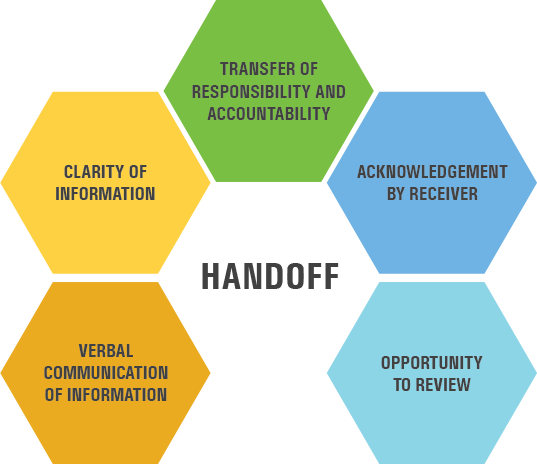
Whenever a patient changes locations or caregivers, a handoff should take place in order to ensure a smooth transition of care. There are several tools and models out there that can help you make a successful handoff, but no matter which tool you use, there should be a concise yet thorough transfer of information with the opportunity to ask clarifying questions and confirm key details. Use a handoff tool to effectively transfer responsibility and accountability for a patient's care.
What is a Handoff?
See It In Action
Keep this in mind....
When it comes to handoffs, consistency is key. Each organization should pick just one handoff tool to use throughout the facility and encourage everyone to implement it.

How do you approach the handoff?

Help Sam and Zoe with a patient handoff.
Handoff Tools
Click through to read about some of the handoff tools available for you to choose from. Each is slightly different with unique advantages, so choose the tool that's best for your team.
I-PASS the BATON
This handoff tool from the TeamSTEPPS curriculum includes additional background about the patient, actions, timing, ownership of care and next steps.
Learn more about I-PASS the BATON.
I-PASS
Stands for: Illness severity (“stable,” “watcher,” or “unstable”); Patient Summary; Action list for the new team; Situation awareness and contingency plans; and Synthesis and "read back" of the information.
This tool has been shown to be particularly effective for physician signout communication and nursing handoffs.
Learn more about the I-PASS tool.
ANTICipate
Stands for: Administrative Data; New clinical information; Tasks to be performed; Illness severity; and Contingency plans for changes.
This handoff tool verifies administrative information, tasks to perform during care and “if-then” contingency plans.
Learn more about ANTICipate.
SHARQ
Stands for: Situation; History; Assessment; Recommendations/Result; and Questions.
Similar to SBAR, SHARQ covers the patient’s situation and history, the sender’s assessment and recommendations and an opportunity for questions at the end.
Learn more about SHARQ.
HAND-IT
The Handoff Intervention Tool follows a checklist-inspired, body system-oriented format to gather and organize information in preparation for a verbal handoff.
Learn more about the HAND-IT tool.
When you pick a tool to use for patient handoffs, let these principles be your guide.
Want to learn more about Project Firstline?
Contact TeamTraining@aha.org.
We value your feedback. Please complete this brief evaluation.


