Boston Medical Center | Massachusetts
Metropolitan Anchor Hospital (MAH) | Case Study
Overview
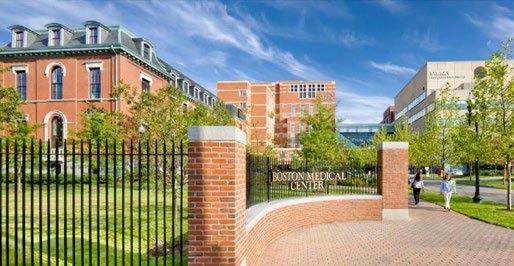 Boston Medical Center (BMC) is a not-for-profit, 514-bed, academic medical center that is the primary teaching affiliate of the Boston University School of Medicine. Dating back to 1855 with the establishment of the Boston University Medical Center Hospital, Boston Medical Center has been driven by a commitment to care for all people, regardless of their ability to pay, providing not only traditional medical care but also programs and services to enhance patients’ overall health. All of this supports its mission to provide exceptional care, without exception.
Boston Medical Center (BMC) is a not-for-profit, 514-bed, academic medical center that is the primary teaching affiliate of the Boston University School of Medicine. Dating back to 1855 with the establishment of the Boston University Medical Center Hospital, Boston Medical Center has been driven by a commitment to care for all people, regardless of their ability to pay, providing not only traditional medical care but also programs and services to enhance patients’ overall health. All of this supports its mission to provide exceptional care, without exception.
In addition to serving as the largest and busiest provider of trauma and emergency services in New England, BMC offers specialized care for complex health problems and is a leading research institution. BMC’s robust research and teaching programs – which train more than 700 residents and fellows each year – keep the hospital on the cutting-edge, while pushing medical care into the future. One recent example: BMC was awarded $89 million in federal funding to lead the NIH HEALing Communities Study with the goal of reducing opioid deaths by 40% in some of the most heavily impacted Massachusetts communities.
Patient–Payer Mix
Boston Medical Center has a long tradition of providing accessible and exceptional care for every patient who comes through its doors. As a metropolitan anchor hospital (MAH), Boston Medical Center faces a challenging patient-payer mix. Even before the pandemic, most of its patients came from historically marginalized communities and had incomes at or below the federal poverty line.
As COVID-19 exacerbated many existing inequities, BMC saw structurally marginalized and at-risk populations increase in its system, with Black, Indigenous, Latinx, and Asian Americans representing 80% of total discharges. In addition, about 20% of patients BMC admitted during the pandemic have been unhoused. BMC’s patients, on average, experience higher rates of chronic disease and tend to have fewer resources to deal with them, leading to worse outcomes and higher health care costs.
“Low-income patients, by definition, end up with more health care challenges – often across many dimensions. Patients come to us with more than just medical needs, so we have to be creative about how to help patients and their families be healthy and stay well. This means addressing the social determinants of health, including access to medication, access to food, and housing insecurity.”
Kate Walsh
President & CEO of Boston Medical Center
Approximately 55% of BMC’s patients are covered by Medicaid or Massachusetts’ Health Safety Net (HSN), and 25% are covered by Medicare. Nearly nine-in-ten visits (86.5%) and more than three-in-four (76.1%) of discharges are from patients covered by Medicare and Medicaid. Yet, just over half (50.9%) of its net patient revenue comes from Medicaid and Medicare. Each year, BMC Health System provides more than $102 million in uncompensated care. MAHs like BMC face significant financial challenges, low margins, and workforce shortages—all of which have been accelerated by the COVID-19 pandemic.
BMC’S Unique Approach to Care
To achieve its goal of making Boston the healthiest urban population in the world, BMC’s leadership has implemented several innovative strategies:
Pivoting from Charity to Equity
BMC has demonstrated a commitment to reducing health disparities with the limited resources it has. For example, BMC has launched the Health Equity Accelerator, which focuses on closing gaps in patient outcomes and transforming care delivery faster using researchers, clinicians, and patient insight.
BMC also operates a wide variety of work, housing, and violence prevention programs — all of which help to keep individuals healthy. Some examples include:
- Recognizing that many patients lack stable housing, BMC invested $6.5 million over five years in affordable housing and related community-based programs – an investment that has spurred similar actions from other local health systems and multiplied the impact.
- To address food insecurity, BMC installed a farm on the roof of one of its buildings, which annually provides over 5,000 pounds of fresh, local produce to hospitalized patients, cafeterias, the Teaching Kitchen, and Preventive Food Pantry, the first hospital-based therapeutic food pantry in the country.
- BMC Pediatrics has a rich history of developing innovative models to address the social determinants of health, many of which have launched as separate non-profit organizations and scaled nationally, including Reach Out and Read, Medical-Legal Partnership, StreetCred, and Health Leads.
Focus on Non-Clinical Outcomes
In addition to focusing on clinical outcomes, BMC strives to understand and improve how patients feel about the care they receive. That is why BMC is working to integrate patient perceptions into its metrics for success. Doing so will help BMC better understand how satisfied patients are with their treatments and identify areas for further improvement.
Metropolitan Anchor Hospitals Need Support
Despite the financial challenges MAHs face, BMC continues to support innovative programs to improve the health and wellbeing of its community. With more stable and equal resources, MAHs like BMC can expand their successful programs, strengthen patient outcomes, and further improve health in their communities.