

Atrium Health Extends Reach with Virtual Care to Improve Health and Elevate Hope

Atrium Health had a head start on leveraging virtual care tools to streamline care when the COVID-19 pandemic hit. It has been a pioneer in the technology tools that support virtual care for more than a decade now.
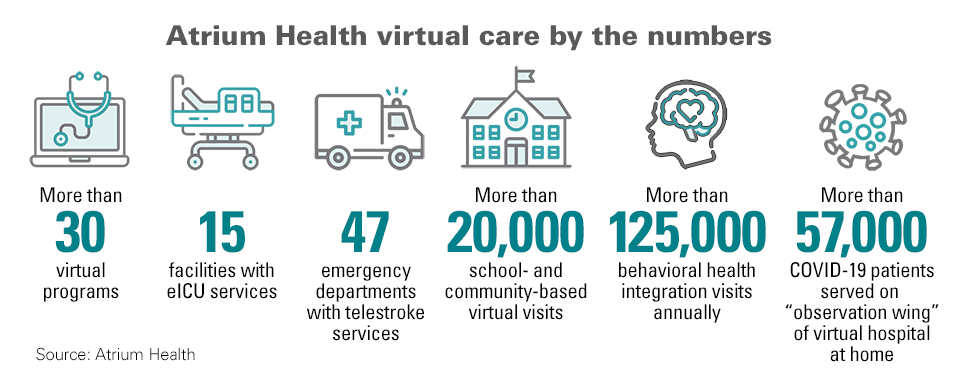
In a recent report, “Transforming Health Care Delivery Through Virtual Care,” Atrium leaders detail how they’ve developed more than 30 virtual programs that streamline access to care, reduce wait times and improve the patient experience. These programs have expanded throughout the medical system to hospitals, schools, community clinics, in-home and on-demand services as well as urgent and primary care settings throughout the Carolinas, Georgia, Alabama and beyond.
Virtual health care at the nonprofit system, part of Advocate Health, is a vital piece of a larger, transformative shift in its entire care model. Katie Kriener, senior vice president of virtual health for Advocate Health and its Southeast region’s medical group operations, notes in the report that technology provides the ability to fulfill the health system’s vision.
Embedding Virtual Care across Operations
Virtual care cuts across Atrium Health’s operations, from hospital at home to school- and community-based virtual health care as well as primary and specialty care. “[We’re] looking at the whole person and creating technical connectivity between patients and providers, between patients and clinicians, improving patient activation with greater, more timely access,” Kriener states.
The numbers illustrate how virtual care permeates the health system’s 40 hospitals and hundreds of care locations.
- 15 facilities have eICU services.
- 47 emergency departments provide telestroke services.
- More than 20,000 school- and community-based virtual visits are conducted annually.
- More than 125,000 behavioral health integration visits are performed yearly, with another 13,700 such visits delivered in emergency departments (EDs).
4 Keys to Atrium Health’s Virtual Care Services
1. Home-Based Care
This flagship virtual care program, one of the largest in the nation, gives patients the option to receive hospital-level care in their homes. With a typical daily census of 35 patients during the summer of 2023, the system intends to be able to care for 200 patients daily in the hospital-at-home model by 2025, says Colleen Hole, vice president of clinical integration and administrator of Atrium Health’s hospital-at-home program.
2. Virtual School- and Community-Based Care
Begun as a pilot program with a single rural school in 2017, the program since has expanded to 150 schools, colleges and community sites, serving more than 20,000 adults and children. The program led to a 32% reduction in preventable ED visits and a 50% return-to-classroom rate when schools reopened after the COVID-19 shutdowns. “After reviewing the outcomes, we proved our hypothesis that by seeing children during the day at school, we could reduce the impact on our emergency departments. It also resulted in more class time for the students and less missed work for parents,” said Lyn Nuse, pediatric primary care medical director at Atrium Health Levine Children’s hospital.
3. Virtual Care in Rural Settings
Technology-enhanced virtual care offerings at Atrium Health Anson include virtual cardiology. Leaders there are also working to establish virtual oncology care, so that a patient can receive a chemotherapy infusion locally under the care of a remote oncologist, without having to drive an hour or more into Charlotte, North Carolina.
4. Virtual Behavioral Health
With a growing need in the community, the health system ramped up its virtual behavioral health programs in all care areas, including hospital, home, school, community and primary care settings. In a dozen acute care hospitals in the system’s Charlotte market, consult teams are available, offering care that is efficient. Care is also available in rural hospitals where there is no psychiatrist on staff. A virtual patient navigation and transition care program allows patients who have been treated in the ED to receive follow-up care at home.



