3 Key Focus Areas to Explore in 2024
Hospitals and health systems have faced unprecedented challenges over the past three years. And now, with the pandemic’s grip on the field lessening, organizations must respond to continuing aftershocks in areas like finance, workforce and evolving care delivery transformation models.
The recently released AHA 2024 Environmental Scan offers a wealth of data and context on these challenges to assist health care leaders in their strategic planning as they reshape the future of health care.
3 Action Areas to Address in 2024
1 | Focus on financial stability.
A confluence of several factors from historic inflation, which is driving up the cost of medical supplies and equipment, to critical workforce shortages, led to 2022 being the most financially challenging year for hospitals since the pandemic began. However, during 2023, hospitals experienced some improvement in financial health. While the median hospital operating margin increased slightly to barely break even, expenses remain high. Additional challenges include Medicaid disenrollment and commercial insurer denials and delayed payments, impacting cash on hand.
Takeaway
Leverage tech solutions to reduce administrative costs. Administrative expenses constitute as much as 31% of overall health care spending, notes an April AHA report; 82% of these costs are attributed to billing and insurance. Look for ways to leverage generative artificial intelligence to alleviate administrative burden throughout the patient journey. A McKinsey & Company report offers these tips to implement the technology.
- Beginning stage of the patient journey: Identify duplicate patient records, automate eligibility determination based on payer policies and contracts, coordinate prior authorizations from health insurance companies and propose solutions to address any administrative gaps.
- Midcycle: Improve clinical documentation accuracy and limit clinicians’ involvement in time-consuming record-keeping.
- End of the journey: Support accounts receivable with automated follow-ups and structure fact-based appeals to health insurers incorporating historical insurer performance, policy manuals and contracted terms.
2 | Hone programs to continue improving quality and safety.
One approach to improving quality of care is through care delivery transformation models. These different models include team-based care, telehealth, alternative sites of care, care at home, addressing societal factors that influence health, and population health management. Value-based payment models serve as a component of a hospital’s operational infrastructure to support these strategies and continue to gain momentum. Private-capital inflows in value-based care assets rose from just 6% in 2019 to 30% in 2021, according to a McKinsey & Company report.
Takeaway
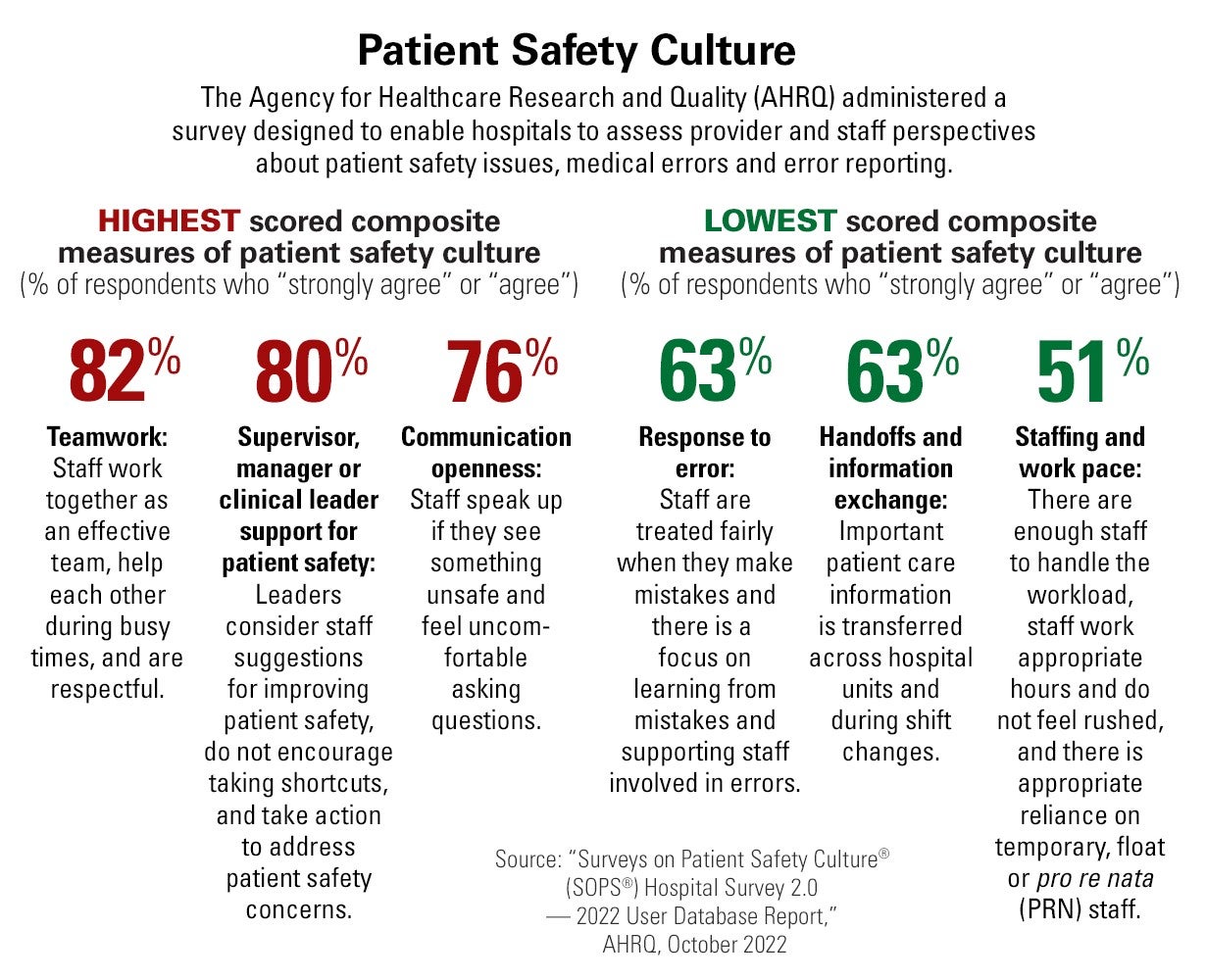
Promote a patient safety culture. As hospitals explore various care delivery models, promoting a culture of safety must remain a constant. An Agency for Healthcare Research and Quality survey report from October 2022 focused on ways hospitals can assess provider and staff perspectives about patient safety issues, medical errors and error reporting. These tables illustrate the highest and lowest composite measures of patient safety culture and areas where provider organizations can explore opportunities for improvement.
3 | Do a deep dive on workforce challenges.
The challenge facing health care is not just a workforce issue, but also a work issue. Organizations need to rethink the work being done by nurses, divide tasks between nurses and technology that augment human capacity and reconsider what work is like when humans and machines work together, notes a research paper co-authored by Kaveh Safavi, M.D., J.D., senior managing director of Accenture’s global health care business. The report notes that as much as 30% of nurses’ tasks can be shifted to automation.
Takeaway
A human-machine mindset could alleviate the nursing shortage. Health care has both a demand and a supply problem. The shortage challenge cannot be solved solely by relying on traditional methods like recruiting, hiring, retention bonuses and flexible scheduling. By introducing technology, reallocating tasks and remodeling nursing jobs, nurses can devote more time to patient care. To explore other ways to address workforce challenges, read AHA’s recently released 2024 Health Care Workforce Scan.



