3 Factors Driving AI Surge in Health Care
Despite the widening deployment of artificial intelligence (AI), its clinical uses remain largely concentrated in areas like diagnostics while applications to streamline business processes are growing.
For hospitals, AI savings come mostly from improvements in clinical operations (improved diagnostic capabilities, operating room optimization) and quality and safety (early identification of patient deterioration, adverse-event detection). With population demands for better access and increased capacity, hospitals also are looking at how technologies like AI can alleviate burdens on staff so they can deliver a better patient experience, improve outcomes and increase clinician satisfaction.
Hackensack Meridian Health recently formed a strategic partnership with Neosoma, a tech company focused on helping clinicians advance the treatment of brain cancers through the use of AI.
The partnership includes clinical data sharing, clinical research and strategic investment from the health system to support Nesoma’s method of imaging, tracking and collecting data on numerous difficult-to-treat brain tumors. Hackensack Meridian physicians will provide feedback for the development of software to be used by neurosurgeons, neuro-oncologists, neuroradiologists, radiation oncologists and others.
Partnerships like this illustrate the rapidly growing AI applications being explored today in health care. Recent research indicates ways hospitals and health systems can leverage AI to improve performance, identify and resolve gaps in health equity, and reduce costs.
3 AI Trends to Keep Your Eye On
Trend 1: Imaging applications explode.
AI’s ability to help discern patterns within data has fueled significant activity in medical imaging and led to a slew of FDA approvals of algorithms for this purpose. Of the more than 520 FDA-cleared AI medical algorithms, nearly 400 are in the radiology field, notes a recent Health Exec report. The next closest algorithms — cardiology (58), hematology (14) and neurology (10) — account for fewer than 100 of market-cleared AI applications, many of which also involve medical imaging.
Takeaway
Explore with your radiology and subspecialty teams AI algorithms that show promise for improving performance and boosting clinical outcomes, including:
- Diagnostic aids that can automatically identify critical findings.
- Automation of time-consuming functions such as quantification, contouring and auto-completion of text in reports.
- Workflow improvements and automation.
- Clinical decision support for next steps in patient care.
- Guidance to help imagers obtain the best possible images regardless of their experience level or if they are unfamiliar with the anatomy.
Trend 2: Nonclinical AI applications expand.
A growing body of research is being incorporated into nontreatment areas to improve processes like note taking, administrative documentation, supply chain and financial management processes.
Takeaway
These operational areas are good starting points for leveraging AI’s power to quickly spot trends so actions can be taken earlier to improve performance and help patients achieve their wellness goals.
Trend 3: AI adoption reduces costs.
While health care is still early in its evolution of adopting AI, the technology’s economic impact on the field could be huge.
Takeaway
Wider AI adoption could save the U.S. 5% to 10% or $200 billion to $360 billion a year, according to research from Harvard University and McKinsey & Company. And while many health care organizations are suffering financially, the value of innovating with technologies like AI cannot be ignored. These estimates are based on specific AI-enabled use cases that employ today’s technologies, are attainable within the next five years and would not sacrifice quality or access.
It May be Time to Talk with Patients about AI
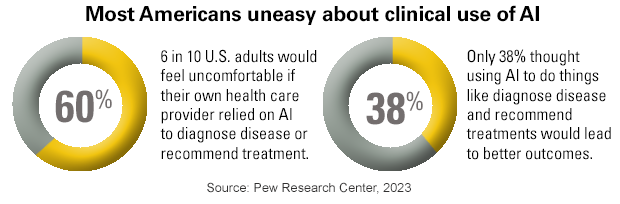
The growing applications for AI in health care have caught the attention of patients. A recent Pew Research survey found that 60% of respondents would feel uncomfortable if their provider relied on AI to diagnose and treat them. Women (66%) were more likely than men (54%) to express concern about AI use in their care. Three-quarters of respondents overall expressed concerns that their providers may implement AI too quickly before fully understanding patient risks.
Connecting with patients on this issue is important to help allay any fears or concerns and to understand fully the nature of patients’ feelings and perceptions. Public awareness of AI in health and medicine is still developing at this early stage.
Pew Research found that Americans make distinctions between the types of applications they are more and less open to. Nearly two-thirds of U.S. adults (65%) say that they would definitely or probably want AI to be used for their own skin cancer screening. Consistent with this view, about half (55%) believe that AI would make skin cancer diagnoses more accurate. By contrast, nearly 80% of the respondents say they would not want to use an AI chatbot if they sought mental health support.



