

Coronavirus Update: CMS Broadens Access to Telehealth during COVID-19 Public Health Emergency
The Centers for Medicare & Medicaid Services (CMS) today announced several waivers and policy changes to broaden access to telehealth services for Medicare beneficiaries during the COVID-19 public health emergency. CMS also released a Frequently Asked Questions document about the changes included in its announcement.
What You Can Do:
Please share this advisory with your executive management team, emergency preparedness staff, billing department and clinical leadership team.
Although CMS provided a number of waivers, the agency did not provide licensure flexibility to allow clinicians to legally provide telehealth services in another state if they have an equivalent license in their home state. The AHA is continuing to stress the challenges caused by this limitation and urging the government to address it immediately. Highlights of the policy changes follow.
Highlights of the policy changes follow under key resources.
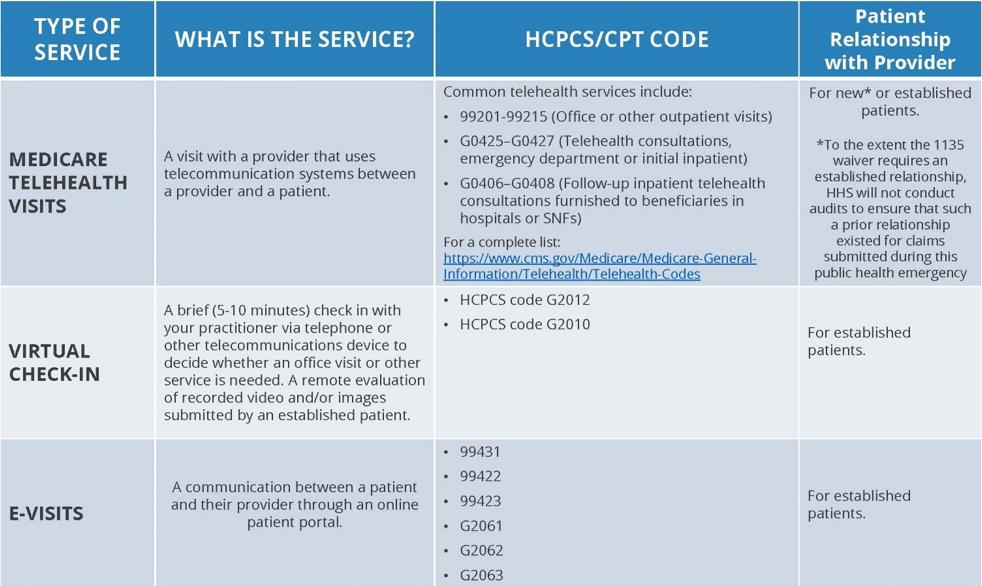
Payment for Medicare Telehealth Services
CMS granted an expanded Section 1135 waiver, under which Medicare will pay for office, hospital, and other visits furnished via telehealth across all areas of the country and in all settings, including in patients’ homes, starting March 6, 2020 and for the duration of the COVID-19 public health emergency. This operationalizes the waiver of the originating and geographic site restrictions on telehealth services that are codified in Section 1834(m) of the Social Security Act (the Act). Medicare considers these telehealth services the same as in-person visits and will pay for them at the same rate as regular, in-person visits.
Cost-sharing
Medicare coinsurance and deductible would generally still apply to the Section 1834(m) Medicare telehealth services, but the Department of Health and Human Services’ (HHS) Office of Inspector General (OIG) is providing flexibility for health care providers to reduce or waive cost-sharing for telehealth visits paid by federal health care programs. More information is available in a policy statement and fact sheet from OIG.
Requirement for Established Patient Relationship
The COVID-19 spending package signed by President Trump last week included “qualified provider” language that limited the delivery of telehealth services to patients with an established relationship with a provider or a member of the provider’s practice. In this announcement, CMS confirms that HHS will not conduct audits to ensure that such a prior relationship existed for claims submitted during this public health emergency.
Virtual Check-ins
In the calendar year 2019 physician fee schedule final rule, CMS established payment for brief, communication technology-based “check-ins” between providers and established patients to determine whether an office visit is necessary. The originating and geographic site restrictions from Section 1834(m) of the Act do not apply to these check-ins and they therefore can be provided in all locations. CMS reminds providers of the availability of these check-ins in this announcement and highlights that providers can use telephones, audio/video devices, secure text messaging, email or use of a patient portal for the purpose of these check-ins. CMS also underscores that patients must agree to individual services but that providers may educate beneficiaries on the availability of the check-in service prior to patient agreement.
E-visits
CMS explains that in all locations and all areas of the country, established Medicare patients may have non-face-to-face patient-initiated communications with their doctors via online patient portals. For these e-visits, the patient must generate the initial inquiry and communications can occur over a 7-day period. Medicare Part B also pays for e-visits or patient-initiated online evaluation and management (E/M) conducted via a patient portal, both with providers who may independently bill Medicare for E/M visits and those who may not (such as physical therapists, occupational therapists, speech language pathologists, and clinical psychologists).
A summary of expanded telehealth authorities appears in the Appendix below.
HIPAA
Effective immediately, the HHS Office for Civil Rights (OCR) will exercise enforcement discretion and waive penalties for HIPAA violations against health care providers that serve patients in good faith through everyday communications technologies, such as FaceTime or Skype, during the COVID-19 nationwide public health emergency. More information is available from HHS.
Condition-agnostic Care
CMS clarifies that the expanded telehealth authority is not limited to patients with or suspected of having COVID-19. Providers may treat patients through telehealth regardless of their diagnosis or symptoms, as long as services are reasonable and necessary.
Appendix
Summary of Medicare Telehealth Services
Key Takeaways
Telehealth flexibilities include
- Waivers of originating and geographic site restrictions on Medicare telehealth services, permitting the delivery of these services in all areas of the country and all locations, including patients’ homes.
- The ability of providers to use expanded telehealth authority for new and established patients for diagnosis and treatment of COVID19, as well as for conditions unrelated to the pandemic.
- Permission for providers to use everyday communications technologies, such as FaceTime or Skype, during the COVID-19 public health emergency, without running afoul of HIPAA penalties.

