MIPS Quality Measurement: Implications for Hospitals and Clinician Partners
The quality payment program (QPP) creates new quality measurement and reporting requirements for eligible clinicians and the hospitals with whom they partner.
However, the QPP’s payment implications will vary depending on a number of scenarios – such as whether a clinician is attributed to the Merit-Based Incentive Payment System (MIPS)i; to a MIPS alternative payment model (APM); or to an advanced APM. See Figure 1. While MIPS-eligible clinicians have a choice of flexible reporting options in 2017 – termed “Pick Your Pace” (see MIPS Overview brief) — they should prepare for potentially expanded reporting requirements in 2018 and beyond.
This brief focuses on MIPS since there are a number of decisions that clinicians need to makeby no later than October 2017 for the first performance year and by Jan. 1 in 2018 and beyond.
Figure 1. MACRA Quality Reporting Scenarios
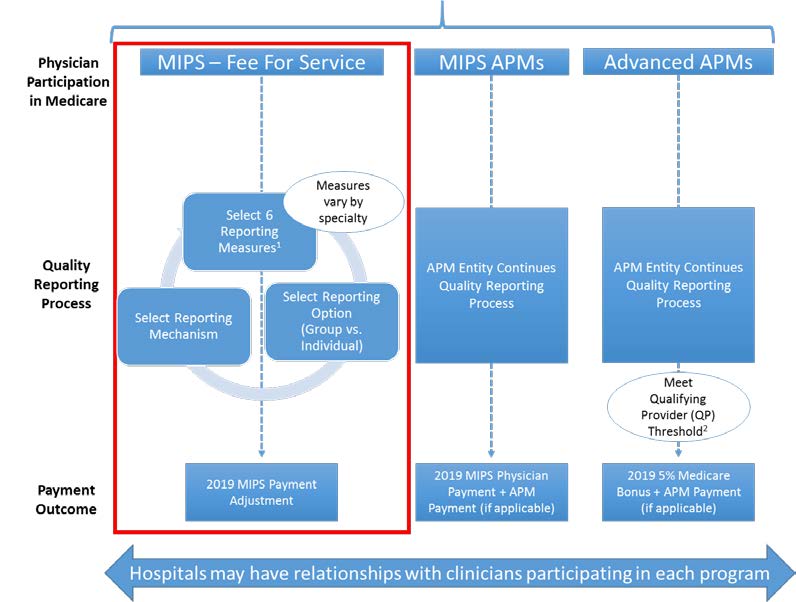
- For 2017, reporting measures should be selected by no later than Oct. 1, 2017 for full-year reporting (to allow for at least 90 days of reporting) and by Jan. 1 for 2018 and for subsequent years.
- Providers that do not meet the QP threshold (for at least 2017) will be scored under the MIPS APM Scoring Standards.
Key Decisions Regarding Quality Reporting and Timelines
To participate in MIPS in 2017 and prepare for full reporting in 2018, eligible clinicians will need to make key decisions that could affect payment, including selecting:
- Quality measures
- Reporting option (i.e., individual versus group reporting)
- Reporting mechanism
Quality Measures. In general, MIPS-eligible clinicians must select and report on six quality measures, but measure availability varies for patient-facing versus non-patient facing clinicians.ii Note that both categories include hospital-based clinicians. See Table 1.
Table 1. MIPS Quality Measure Requirements
|
Patient-Facing Clinicians |
Non-Patient Facing Clinicians |
|
Requirements: • Choose and report on six measures selected from an individual or specialty measure set. • One must be an outcome measure or high priority measure (if a relevant outcome measure does not exist for the individual clinician or group) • Specialists can select six individual measures or a specialty measures set. If specialty set is fewer than six measures, report all measures in set Resources • Searchable list on CMS Quality Payment Program website • MACRA QPP Final Rule o Table A: Finalized Individual Measures in 2017, p. 77558 o Table E: Finalized 2017 Specialty Measure Sets, p. 77686 |
• Same general requirements as patient-facing clinicians apply. Several policies aimed at helping non-patient facing clinicians, such as: o Reporting on specialty specific measure sets, which could have fewer than the required six measures o Report through a QCDR, which can report non-MIPS measures |
In additional to the six selected measures, quality performance will include a population health measures (the all-cause readmission measure for 2017), which CMS will automatically calculate and apply to groups of 16 or more clinicians who have a case volume of 200 cases. Performance on the All-Cause Readmission measure will not be applied to solo clinicians or groups of 15 or less (see Table B: Quality Measures That Are Calculated for 2017 MIPS Performance That Do Not Require Data Submission, p. 77675). Measure selection should also consider the opportunity for bonus points by selecting high priority measures— outcome, appropriate use, patient safety, efficiency, patient experience and care coordination measures.
Reporting Options. MIPS-eligible clinicians must decide if they will report as individuals or as a group. This will affect their choices for reporting mechanisms as well as their MIPS score, which determines payment.
Reporting Mechanisms. Clinicians can select from a number of reporting mechanisms depending on whether they are reporting as an individual or group. See Table 2.iii Hospitals and clinicians may already have some of these reporting mechanisms in place; for example, clinicians participating in the Physician Quality Reporting System may already use a qualified clinical data registry (QCDR) with support from a hospital. For hospitals contracting with vendors, note that vendors may not be able to support all quality measures, so it will be important to assess vendor capabilities to support MIPS quality reporting.
- Individual reporting and scoring will be based on a combination of the individual clinician’s tax identification number and national provider identifier (TIN/NPI)
- Group reporting and scoring will be under one billing TIN. A group is defined by a TIN with two or more MIPS-eligible clinicians, as identified by their individual NPI, who have reassigned their billing rights to the TIN. Note that not all reported measures may apply to all clinicians in a group.
Table 2. Quality Data Reporting Mechanisms Available Under MIPS
|
Individual |
Group |
|
• QCDR • Qualified Registry • EHR • Claims |
• QCDR • Qualified Registry • EHR • CMS Web Interface (groups of 25 or more) • CAHPS for MIPS Survey (Must be reported in conjunction with another data submission mechanism) • Administrative Claims (For all-cause hospital readmission measure; no submission required) |
Table 3—Data Submission Mechanism for MIPS Eligible Clinicians Reporting Individually As TIN/NPI, and Table 4—Data Submission Mechanism for Groups, p. 77094-5, Federal Register, Vol. 81, No. 214, Friday, November 4, 2016
Generally, groups do not need to register to report selected measures using a third-party entity except if they are submitting:
- Data on performance measures via the CMS Web Interface, or
- Reporting the Consumer Assessment of Healthcare Providers and Systems (CAHPS) for MIPS survey
Registration for these two exceptions must occur by June 30 of the performance period.
i In year 1 and 2, eligible clinicians will include physicians, physician assistants, nurse practitioners, clinical nurse specialists and certified registered nurse anesthetists. The Secretary of HHS has the option to expand the list in year 3 of the program.
ii In general, a non-patient facing clinician is one whose day-to-day work does not involve direct patient interaction (for example, a pathologist based in a lab, a radiologist interpreting images).
iii Submission criteria for group and individual reporting under MIPS, available in Table 3—Data Submission Mechanism for MIPS Eligible Clinicians Reporting Individually As TIN/NPI, and Table 4—Data Submission Mechanism for Groups, p. 77094-5, Federal Register, Vol. 81, No. 214, Friday, Nov. 4, 2016.

