Fact Sheet: Reset IMPACT Act to Account for COVID-19 Lessons on Post-acute Care
Updated April 28, 2021
The Issue
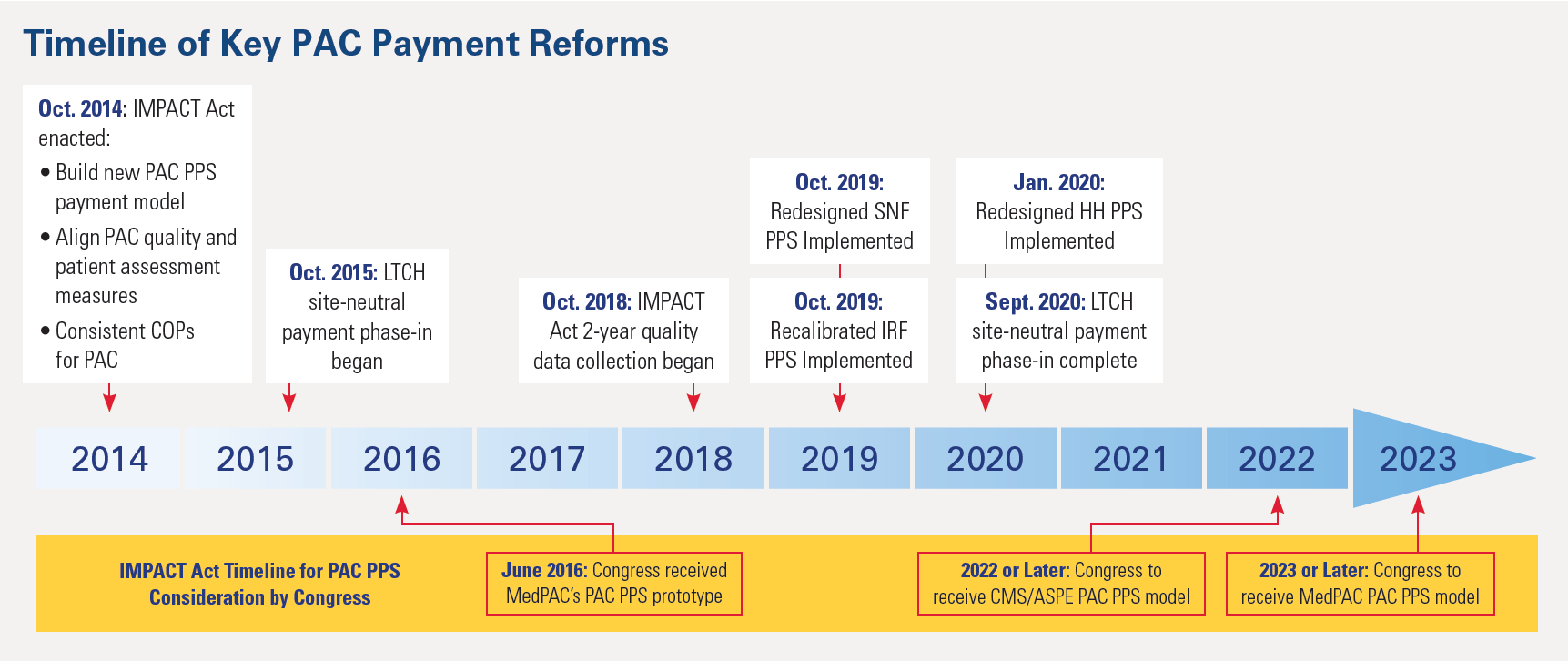
The Improving Medicare Post-Acute Care Transformation (IMPACT) Act of 2014 was enacted, in part, to modernize payments, for the four post-acute care (PAC) settings: home health (HH) agencies, skilled nursing facilities (SNFs), inpatient rehabilitation facilities (IRFs) and long-term care hospitals (LTCHs). However, the legislation could not account for the transformative changes implemented following its passage, much less the COVID-19 pandemic. To make the IMPACT Act relevant to the current PAC landscape, the law must be updated to align with recent transformations of the existing PAC payment systems, as well as to recognize the COVID-19 pandemic, which continues to require extraordinary action by providers across the continuum of care, including PAC. Patient data collected before these payment reforms and during the pandemic could distort the payment accuracy of a unified PAC payment model. A refresh of the IMPACT Act mandate is critically important.
PAC Role in COVID-19 Response
- COVID-19 continues to place an unprecedented strain on the entire health care system, including PAC providers. All four PAC settings are treating patients with active COVID-19, as well as patients recovering from the virus – albeit patients with different levels of acuity and medical needs. In addition, referring hospitals, to create more space for those affected by the virus, are transferring patients to PAC facilities that correspond with the needed clinical competencies.
- Services for these pandemic-affected patients have both highlighted PAC strengths and materially altered operations in ways that affect the scope and cost of PAC care – shifts that should be exempted from the new payment model. For example, during the public health emergency, PAC providers treating high-acuity patients with or recovering from COVID-19 have experienced greater costs per patient due to their need for isolation care, high-concentration oxygen, extra physician and respiratory therapist services, patient protective equipment, and other COVID-19-specific resources. Further, for some PAC providers, average acuity levels have risen due to case-mix shifts in referring hospitals, which affect the downstream PAC patient mix, especially during virus surges. Collectively, these pandemic-driven shifts affect the patient assessment data in ways that are unique to the public health emergency, and, if not excluded, would distort the payment accuracy of a unified PAC payment model.
Resetting the IMPACT Act
The PAC prospective payment system development mandate and timeline established in the IMPACT Act, outlined below, must be immediately revisited and reset to reflect 2021 realities. The Resetting the Impact Act (TRIA) of 2021 (H.R. 2455) would accomplish this goal by excluding from the new payment system prototype the data collected both prior to the recent PAC payment systems’ reforms as well as during the COVID-19 pandemic. Without these exemptions, the prototype will not reflect the post-pandemic resource needs of certain PAC patients – most likely those with medical complexities – with resulting payment inaccuracies that would create access challenges for affected patients.
Ongoing PAC Payment Reforms
- HH Reform. In January 2020, a reengineered HH payment system was implemented, the patient-driven groupings model, which shifts resources from high-therapy to medically complex patients.
- SNF Reform. In October 2019, a completely redesigned payment system was implemented for SNFs, the patient-driven payment model, which shifts resources from high-therapy to medically complex patients.
- LTCH Reform. In October 2015, the LTCH field launched a two-tiered payment model that pays far lower rates for lower-acuity hospital patients, now 1 out of 4 cases. This reform – which was recently fully implemented – continues to reduce overall LTCH volume and yield LTCH closures.
*Conditions of participation
*Centers for Medicare & Medicaid Services
*Office of the Assistant Secretary for Planning and Evaluation

