AdventHealth Physician, Team Pioneer Endoscopic Procedure Allowing Patient to Eat Again
Rene Galloway is no stranger to patient care. As a former nurse, she spent many shifts caring for patients in the emergency department at AdventHealth Celebration. Unfortunately, health struggles resulting from gastric bypass surgery led to nine additional surgeries over 13 years, and left her with no choice but to receive intermittent nourishment through an IV.
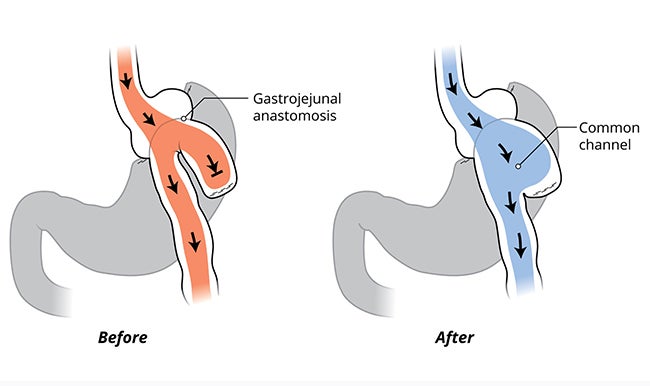
Candy cane syndrome refers to patients, like Galloway, who have undergone gastric bypass and develop significant and sometimes debilitating abdominal discomfort due to the small bowel taking on a hook shape, similar to the end of a candy cane. Symptoms typically begin after eating and can often only be relieved by vomiting.

“There’s been a fear of eating because it was painful, and I never knew when I would vomit,” said Galloway.
When told by other physicians that she was not a good candidate for corrective procedures, gastroenterologist Kamibiz Kadkhodayan, M.D., (Dr. K.), at AdventHealth’s Center for Interventional Endoscopy became her last resort.
Multidisciplinary approach leads to groundbreaking surgery

“When Dr. K. came into the room, he sat down and took the time to sketch these drawings detailing the surgery and how he was going to help me,” Galloway said. “I’ve never seen that from a physician, and my husband and I had tears in our eyes because we knew Dr. K. could give me my life back.”
Galloway became the first in the world to have a brand-new procedure, endoscopic blind limb reduction with septotomy — dubbed the “candy cane” procedure — developed and performed by Dr. K and the AdventHealth care team.
Dr. K. and his team were able to treat Galloway’s condition with no incisions. First, they worked to reduce the size of the hooked portion of the bowel using a repurposed endoscopic device, and then followed with a second procedure that created a channel for food.
“We were able to repurpose FDA-approved gastroenterologist tools to achieve a procedure similar to surgery but less invasive,” said Dr. K. “By suturing endoscopically and dissecting with the use of electricity, we were able to reduce the blind pouch.”
Dr. K credits the multidisciplinary approach at AdventHealth for the success of the groundbreaking surgery. Having various subspecialities all sitting together at the table discussing Galloway’s situation allowed for more innovation. The results improved her life — and also have changed the course of treatment for future patients.
Successful treatment inspires life changes for patient
To say the past several months have been life-changing for Galloway would be an understatement. When she came to AdventHealth for her first surgery, Galloway had been on IV nutrition for about three months because she couldn’t always keep food down. After her procedure, she left the hospital and ate her first meal, savoring every bite. She has been able to eat without issue ever since.
“I don’t have to keep nausea medicine and grocery bags on hand anymore in case I get sick,” said Galloway. This surgery has allowed me to go back to work full time and spend time with my family again. I can now go out to restaurants and have family dinners and beach days again.”
It’s been a long, sometimes painful journey for Galloway since her first gastric bypass surgery in 2009, but she’s now able to get back to her daily life, thanks to this innovative surgery. She hopes to be the model patient by adopting a healthier lifestyle, eating the right foods and exercising to fully enjoy her second lease on life.
“Dr. K gave me hope. This surgery has given me my life back,” said Galloway.