

3 Ways to Strengthen Physical and Behavioral Health Integration
As hospital and health leaders continue to seek sustainable solutions to address workforce shortages, negative margins and rising labor costs, they may want to take a deeper look at ways to integrate physical and behavioral health services.
At least six positive impacts can be achieved by integrating these two areas of care delivery, notes a recent AHA Issues Brief, “Integrating Physical and Behavioral Health: The Time Is Now.” The benefits include:
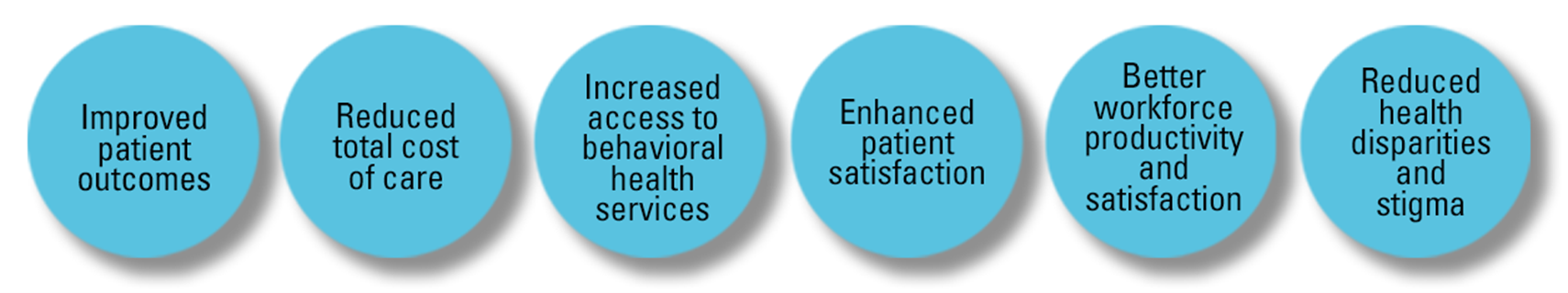
The Value of Delivering Integrated Care
Integrating the treatment of physical medical and behavioral health disorders within the primary care setting can improve health and well-being. Part of whole-person care, integrated health care is a rapidly emerging shift in the practice of high-quality health care, according to the Agency for Healthcare Research and Quality (AHRQ).
This is a critical issue given that 70% of patients with behavioral health disorders have a medical co-morbidity, while at least 30% of adults with a physical condition also have a behavioral health disorder.
Integrated care delivery is associated with broad improvements in symptoms, functioning and well-being, as well as improved management of chronic conditions, decreased hospitalizations and emergency department (ED) visits, and improved overall quality of life for patients.
3 Ways to Strengthen Physical and Behavioral Health Integration
1 | Support physicians as they integrate care.
The American Medical Association and seven other leading medical associations have established the Behavioral Health Integration Collaborative, a group dedicated to catalyzing effective and sustainable integration of behavioral and mental health care into physician practices. The collaborative has created behavioral health how-to guides to give physicians actionable, evidence-based strategies for integrating physical and mental health care.
2 | Identify the best ways for your organization to integrate care.
Co-locate, embed or even provide access to behavioral health clinicians via telehealth (including by phone) in a primary care physician’s office to improve timely access to behavioral health care. And wider access to care also may help lessen the stigma of seeking behavioral health services, all while improving access.
3 | Educate the community on the new whole health services.
Patients like the convenience of being able to access physical and behavioral health services in one setting with which they are familiar, AHRQ states. Moreover, when behavioral health clinicians are embedded in primary care clinics, it allows for an in-person handoff between two care team members. So, inform your community of the value-added services you now offer.
3 Benefits to Integrating Behavioral and Physical Care
1 | Lower Total Cost of Care
Even before the pandemic, one out of four admissions to a general acute care hospital involved a co-morbid behavioral health disorder. Research shows that total health care costs are 75% higher for people with co-existing behavioral and physical health conditions than for those without a behavioral health issue. Yale New Haven research found that implementing a particular integrated behavioral health model resulted in a 159% return on investment, with every dollar invested in the program delivering $1.70 to the organization. A Western New York study of six primary care practices found that integration reduced ED visits by 14.2%.
2 | Better Workforce Productivity and Satisfaction
The University of Michigan’s Behavioral Health Workforce Research Center found that integrated care can have a positive impact on staff by increasing employee productivity, boosting employee satisfaction and stabilizing primary care physicians’ workload, enabling them to more easily refer patients to other specialties where they may lack expertise. A 2022 study of the collaborative care model (CoCM) of integrations showed an increase in provider satisfaction and provider confidence in managing behavioral health problems.
3 | Greater Reimbursement Opportunities
Key findings from a recent report by American Health Insurance Plans found that employer-coverage and individual market plans increased payment to the CoCM and Behavioral Health Integration codes in 2018-2021 by an average of 18%. Meanwhile, providers’ use of these codes in commercial markets increased nineteenfold during the same period.
Learn More
This AHA news story features new case studies on the importance of integrating physical and behavioral health. Also, read the AHA Bipartisan Policy report, “Achieving Behavioral Health Care Integration in Rural America” for information on the value of providing integrated care in rural areas.ICYMI: More Behavioral Health Resources
 Fast Facts: 2023 Behavioral Health Infographic
Fast Facts: 2023 Behavioral Health Infographic
A new Fast Facts infographic on behavioral health provides statistics on the number of psychiatric and other behavioral health hospitals and hospital services in the U.S. Included is trend data on hospitals providing psychiatric screenings and on hospitals that are consulting/liaising behavioral health care with acute inpatient care, emergency services and more. Download the infographic.
 Behavioral Health Integration: Treating the Whole Person
Behavioral Health Integration: Treating the Whole Person
Behavioral health disorders have significant impact on individual and community health, utilization of services and costs. Hospitals are shifting their focus to treating the whole patient and creating a continuum of care that reflects integration at each point in a patient’s journey to better health. This means integrating behavioral health services into every aspect of patient care. Download the report.



