

Executive Burnout Is Real — and It Can Be Reduced

In times of crisis, health care leaders need to be at their best. Throughout the pandemic, hospital and health system executives have demonstrated that ability. But the pandemic’s duration, shifting regulations and reimbursement rules, financial pressures, staff shortages and other factors are taking their toll on C-suite executives.
Nearly three-quarters of health care executives say they have felt burned out in the last six months and 93% believe burnout is negatively impacting their organizations, according to a recently published WittKieffer survey.
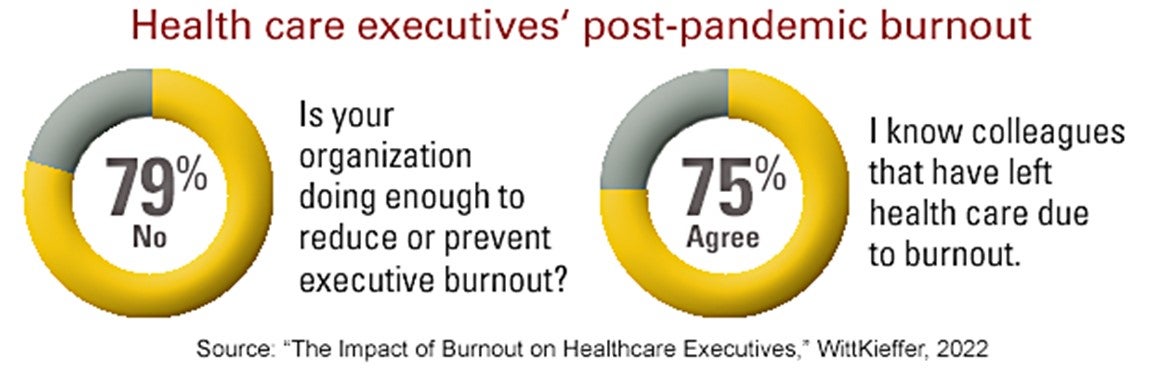
Indicating more can be done, 79% of the respondents said their organizations aren’t doing enough to reduce or prevent executive burnout. While more than half said their employers offer some kind of service or benefit — and in some cases more than one option — as a means of preventing or reducing burnout, some said no services are offered.
The survey, which included responses from 343 CEOs, chief financial officers, chief medical officers, chief nursing officers and other C-suite executives at the vice president and director levels, was conducted this past summer.
The Impacts of Executive Burnout
Those reporting feeling burned out are much less hopeful about the future of health care leadership, feel significantly less productive at work and less determined to make an impact in their work and careers. Other data show similarly concerning trends.
- 75% know colleagues that have left health care due to burnout.
- 51% say burnout could cause them to leave their positions.
- 50% say burnout could cause them to look at positions outside health care.*
“I think that burnout has become the new norm in health care because of increased financial pressures over the past several years. Many organizations have taken the ‘do more with less’ approach to the extreme and I think talented leaders are leaving health care because of it,” one executive respondent notes.
Seventy-one percent of respondents say they are concerned that burnout will affect their careers in health care management. The percentage was just under 60% among those who felt burned out in the last six months, but it’s clear that the stresses brought on by the current health care landscape are having a detrimental impact on many leaders.
While seemingly split on whether burnout prevents them from doing their best work, most respondents believe there is more work to do than they can accomplish.
Burnout Follows Leaders Home
Not surprisingly, many leaders feel that the effects of burnout are impacting their lives outside the office.
- 65% report rarely or never taking all their allotted vacation days due to their workload.
- 56% aren’t getting seven to eight hours of sleep per night.
- 47% say burnout has had a negative impact on their personal relationships.
- 46% frequently skip at least one meal per day because they are too busy or stressed from work.*
Despite these impacts, some executives conclude in written comments that it’s all part of the job, albeit that the job has grown more challenging over the last several years as financial pressures on organizations have mounted significantly. Many remain optimistic that the impacts of burnout can be managed by taking proactive steps.
“I think we need to consider how to build resilience and take a positive spin on how to build a healthy life balance,” one respondent notes.
5 Ways to Address Burnout
1 | Measure burnout rate.
Identifying the issue is the first step and action should swiftly follow. Organizations should openly address the topic and encourage proactive conversation before things become unsalvageable.
2 | Build more efficient work teams.
Noted by 26% of the respondents, this could help improve operating efficiency and workflows.
3 | Adjust expectations and deadlines.
Maintain a strategic focus and say “no” to the nonessential tasks and requests for time.
4 | Improve alignment on top priorities.
Define how your team will measure success, scope of roles and improve clarity and transparency on decision-making processes. This will help with team connectedness and support for the leadership vision.
5 | Don’t be afraid to step away.
Using vacation time to recharge is essential. Spending time with family and friends and engaging in a favorite hobby were the top suggestions among respondents to reduce or prevent career burnout. Any activity — working out, yoga, spending time alone reading or praying — that helps you refresh is worthwhile.
Learn More
The following AHA leadership resources can help support leadership teams in creating a new professional strategy to offset the demands of the 24/7/365, fast-paced and unrelenting health care environment.
AHA Leadership Experience 2023
This program helps participants develop a powerful ability to develop new skills, patterns and rituals that create equilibrium among the competing dimensions of their lives.
AHA Next Gen Leaders Fellowship
This annual program is a unique opportunity for developing leaders to bring about change in the hospital and health systems in which they serve. Each Fellow is paired with an executive-level mentor who will guide them through the planning and execution of a yearlong project.
AONL educational programs
The American Organization for Nursing Leadership offers virtual and in-person programs to expand the leadership skills of nurse managers.
Update
As we noted in this December 20 lead story, the past few years have taken a heavy emotional toll on health care executives. A recent WittKieffer report provides details about this issue.
In our story about findings from the report, we inadvertently included some data from WittKieffer’s 2018 report that addressed this subject as well. To clarify, see the complete results for the 2022 WittKieffer report.



