

Market Expands for Teaching Value-Based Care Imperatives
 />
/>
What’s New
Utah-based Intermountain Healthcare recently spun off a new company, Castell, to help providers and payers accelerate their transition to value-based care.
The nonprofit company will share best practices from Intermountain’s prevention-focused Reimagined Primary Care delivery model and offer a technology and analytics platform to guide care. Castell also will provide digital tools for virtual care, patient experience and social determinants of health, as well as provide access to Intermountain’s latest innovation initiatives.
In its first year, the Reimagined Primary Care model has led to:
- A 60% cut in Medicare Advantage admissions.
- 25% fewer commercial insurance admissions.
- A 20% reduction in per member per month costs.
- Improved patient ratings and physician satisfaction.
What’s Going On
Intermountain is leveraging its deep knowledge in improving quality, reducing costs and effectively managing downside risk in value-based care programs to improve access. Its leaders say they are shifting to a more community-based mindset and that Castell will provide benefits to adjacent markets in Utah and Nevada. This could help participating providers in these areas to improve efficiency and outcomes and cut costs as they participate in value-based care models.
The launch of Castell also is part of a broader trend among some health systems to diversify their business lines outside of reimbursable medical services. These innovators are creating companies in areas like technology, automation, group purchasing and supply chain management. And with the field likely being several years or more away from assuming full risk in value-based payment models, others are stepping up with services to help ease the transition.
Providence St. Joseph Health, for instance, earlier this year launched Ayin Health Solutions, a population health company that offers expertise to help payers, providers, employers and government entities reduce costs and improve care in the transition from inpatient to ambulatory care. Evolent Health, an independent company formed by UPMC and The Advisory Board in 2011 to provide an integrated population and health management platform, is a $1 billion company today focusing on helping providers and health plans succeed in value-based care. Among its partners are Banner Health Network, Passport Health Plan, St. Luke’s Health Partners and Deaconess Health System.
 If You Build It, Will They Come?
If You Build It, Will They Come?
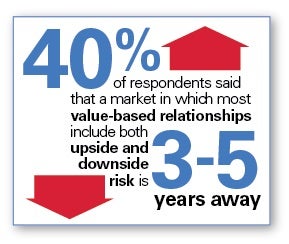
Whether these latest business launches will have the staying power of Evolent Health remains to be seen, but many providers are looking for insights and tools as they move deeper into value-based care. However, it could be some time before the bulk of the field assumes full risk in value-based payment models, as a HealthCare Executive Group and Change Healthcare survey of health care executives found earlier this year. The study noted that nearly 40% of respondents said that a market in which most value-based relationships include both upside and downside risk is three to five years off.



