Affordability Advocacy Agenda
The American Hospital Association continues to incorporate principles that promote improved value into our ongoing policy and advocacy activities.
September 2022
Advancing Affordability, Value, and Equity in Health Care Priorities for America’s Hospitals and Health Systems
By all accounts 2020 was an unprecedented and historic year – one that tested our nation, our economy and our health care system like never before.
Hospitals, health systems and post-acute care providers – along with our doctors, nurses and other team members – have been on the front lines of the COVID-19 pandemic, working tirelessly to provide the best care for patients, families and communities. They have done this – and continue to do this – while facing daunting challenges. These challenges have persisted well into 2021, with continued surges of cases and hospitalizations.
At the same time, individuals, employers, and the government continue to seek greater value for their health care dollars. Concerns around the affordability of health care will only grow as overall health care spending continues to rise and, especially with respect to publicly-financed programs like Medicare and Medicaid, demographic trends mean that there are fewer workers to help finance this care. There is also a renewed focus on eliminating disparities in care, closing equity gaps, and enhancing quality and patient safety – all of which are integral to achieving greater value.
Our shared focus with Congress and Administration is on providing relief from the pandemic, ensuring a smooth recovery, and rebuilding a better health care system for the future. The American Hospital Association continues to incorporate principles that promote improved affordability, value, and equity into our policy and advocacy activities. Below are some of our key priorities in these areas.
Making Health Care More Affordable
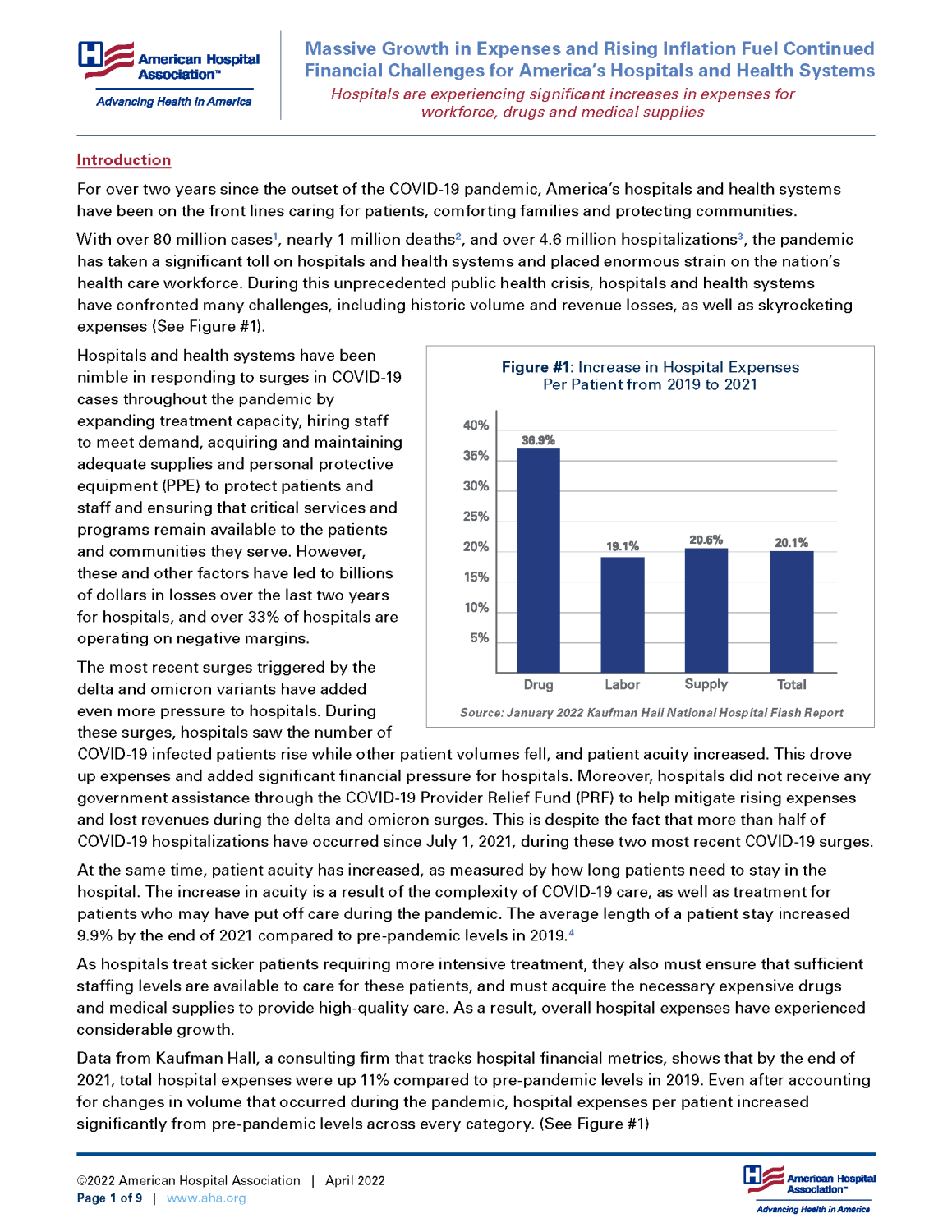
In recent years, health care spending growth has largely been driven by increased use and intensity of services. In other words, more people are getting care – and more care – and the care they are getting is more involved than in the past. Much of this is the result of substantial expansions in health care coverage, improved efforts to connect people to needed care, advances in medicine and technology, and growth in the prevalence of chronic disease. In some cases, prices have also risen, such as for prescription drugs. This can impact not only what individuals may pay at the pharmacy counter but also the cost of care provided by hospitals, physicians, and other providers that relies on critical drug therapies. Another substantial cost driver that has dramatically escalated in the past several years is the utilization management processes that health plans have erected and which require significant investments in technology and personnel to manage.
Hospital care requires a range of inputs such as wages for clinical and other personnel, prescription drugs, administrative software and other technology, food, medical devices, utilities and professional insurance. Steep increases in the prices for certain inputs, like drugs and administrative processes mandated by health plans, can undermine hospitals’ efforts to reduce the cost of care.
To address the underlying cost drivers in the health care system, we urge Congress and the Administration to:
- Rein in the rising cost of drugs, including by taking steps to increase competition among drug manufacturers; improve transparency in drug pricing; and advance value-based payment models for drugs.
- In the same vein, protect the 340B drug savings program to ensure structurally marginalized communities have access to more affordable drug therapies by reversing harmful policies and holding drug manufacturers accountable to the rules of the program, especially as it relates to community pharmacy arrangements.
- Reduce administrative waste by streamlining prior authorization requirements and processes for hospitals and post-acute care providers, so that clinicians can spend more of their time and resources on direct patient care, not pushing paper and arguing with insurance companies over administrative delays and coverage denials.
- Promote greater efficiency and safeguards against unnecessary burden in HIPAA administrative standards and other rules related to billing and ensure an achievable roadmap toward greater adoption of standard transactions.
- Reduce unnecessary costs in the system by passing comprehensive medical liability reform, including caps on non-economic damages and allowing courts to limit attorneys’ contingency fees.
Improving the Affordability of Coverage
In addition, we urge Congress and the Administration to take additional steps to make health care coverage more affordable and easier to use for patients. The entire point of insurance is to share large and unanticipated costs across a pool of people. Coverage is essential for making health care affordable for individuals and families in the same way car insurance enables individual drivers to weather the bad fortune of an unexpected crash. While we have made substantial gains in health coverage over the past decade, we are just beginning to fully understand the crisis of under-insurance that is primarily being driven by high deductible health plans.
The AHA supports bolstering our current public/private framework for coverage to close the remaining coverage gaps and taking immediate steps to ensure that patients do not face financial barriers to using their coverage. We encourage policymakers to preserve and build on the strong foundation of employer-sponsored coverage and further strengthen the individual market while ensuring that Medicare and Medicaid are available to those who rely on these programs. Specifically, we encourage Congress and the Administration to:
- Take additional steps to close coverage gaps, including by building on the existing incentives to encourage all states to expand Medicaid, making permanent the recent expansions in eligibility and the level of subsidies for coverage on the Health Insurance Marketplaces, and expanding existing outreach and enrollment efforts to ensure that every U.S. resident knows their options for coverage.
- End the sale of products purporting to be health plans but that do not meet all of the consumer protections established in federal law, such as health sharing ministries and short-term limited duration coverage products which can leave patients with high and unexpected medical bills as a result of gaps in coverage.
- Restrict the sale of high deductible health plans to consumers who can afford the associated cost-sharing obligations.
- Ensure patients can rely on their coverage by disallowing health plans from inappropriately delaying and denying care, including by making mid-year coverage changes.
- Protect patients from surprise medical bills and ensure that the implementing regulations do not unintentionally distort health care markets and reduce patient access to care.
- Support price transparency efforts by ensuring patients have access to the information they seek when preparing for care, including cost estimates when appropriate, and creating alignment of federal price transparency requirements to avoid patient confusion and overly burdensome duplication of efforts.
Advancing Value through Health System Transformation and Enhancements in Quality
Health System Transformation
In addition to making the health care system more affordable, hospitals and health systems are committed to ensuring that each dollar brings value. We will achieve this by continuously striving to deliver the highest quality care most efficiently, and that will require rethinking how and where we deliver care. We will also look for opportunities for providers to collaborate with payers and employers to ensure aligned incentives to achieve value, including identifying effective models of risk where appropriate.
The last decade brought significant changes in the health care landscape, but nothing has accelerated changes in the delivery of health care like the COVID-19 pandemic. During the public health emergency, hospitals and health systems were able to innovate at a pace and scale previously unseen as a result not only of the realities of containing a pandemic but also the regulatory flexibility provided by states and the federal government.
The AHA is eager to continue these advances and supports policies that:
- Expand use of telehealth, broadband and digital technologies by providing Medicare and Federal Communications Commission funding, coverage, and reimbursement for such services, technology and workforce training.
- Implement policies to better integrate and coordinate behavioral health services with physical health services.
- Build on the progress in modernizing the Stark Law and Anti-kickback Statute regulations that better protect arrangements that promote value-based care.
- Allow providers to determine how best to utilize electronic health records (EHRs) and other technologies while promoting interoperability and access to health information for clinical care and patient engagement.
- Provide robust support to ensure electronic communication between acute care hospitals and psychiatric hospitals and providers, and to encourage psychiatric hospitals and mental health providers to optimally use EHRs.
- Advance use of innovative technologies and software (e.g., clinical decision support algorithms) without increasing regulatory burden by supporting policies that enable clinicians to have the data they need to treat patients and improve health outcomes.
- Invest in health care infrastructure by expanding access to virtual care technologies and high-speed internet, strengthening the capacity and capability for emergency preparedness and response, assisting hospitals in “right-sizing” to meet the needs of their communities, and ensuring adequate financing mechanisms are in place for hospitals and health systems, including for training the workforce.
- Address the impact that social determinants of health have on patient outcomes by improving care coordination and expanding the tools hospitals can use to meet these needs.
- Advance rural health care alternatives to ensure sustainable care delivery and financing including: exploring rural pre-payment models; supporting additional inpatient/outpatient transformation strategies; promoting virtual care strategies; allowing innovative partnerships; and refining existing models that support hospitals serving historically marginalized communities.
- Explore a new payment mechanism for metropolitan anchor institutions that treat a disproportionate number of government-funded or uninsured patients.
Enhancing Quality and Patient Safety
America’s hospitals and health systems are world-renowned for the quality of care they provide and are always striving to do even better. Clinicians at U.S. hospitals set the global standard in COVID-19 care, such as by optimizing the use of ventilators for those patients who would most benefit from them. – knowledge that was then shared around the world.
There is no limit to hospitals’ and health systems’ commitment to quality. However, policy changes are needed to facilitate the identification and adoption of best clinical practices, including addressing challenges with public quality reporting and incentive programs. The AHA encourages policymakers to:
- Continue to streamline and coordinate quality measures in national programs to focus on the “measures that matter” most to improving health and outcomes while reducing burden on providers. These measures should be based on evidence that demonstrates meaningful improvements in patient outcomes are achievable by improving adherence to the measures.
- Advocate for modernized conditions of participation, interpretative guidance and Joint Commission standards that hold hospitals accountable for taking actions that lead to higher-quality and safer care.
- Enhance the effectiveness of the physician quality payment program by advocating for more accurate and meaningful cost measures and data-driven implementation of new program approaches.
- Promote advanced illness management to better honor patients’ wishes at the end-of-life and remove barriers to expanding access to palliative care services.
- Enhance care coordination and improve patient safety by implementing through rulemaking Sec. 3221 of the Coronavirus Aid, Relief, and Economic Security (CARES) Act, which revises and better aligns the outdated 42 CFR Part 2 regulations with HIPAA, allowing the responsible sharing of substance use disorder treatment records for the purposes of treatment, payment and health care operations.
Advancing Health Equity, Eliminating Health Care Disparities, and Increasing Diversity and Inclusion
The COVID-19 outbreak in the U.S. has shown the country what all hospital and health systems leaders have known for years: serious gaps exist in access, cost and quality for patients based on race, ethnicity, gender and gender identity, age, sexual orientation or other demographic and socio-economic factors. Hospitals and health systems are committed to doing the work to address health equity issues. The AHA and its Institute for Diversity and Health Equity (IFDHE) are also committed to advancing health equity, eliminating health care disparities and increasing diversity and inclusion. The AHA supports policies that:
- Pursue strategies and support public policies aimed at improving maternal and child health outcomes with a particular focus on eliminating racial and ethnic disparities.
- Promote health equity by encouraging cultural humility training in medical residency programs and in-service training for health care professionals.
- Promote inclusion of adjustment for sociodemographic factors in quality measurement programs where appropriate to ensure performance measurement and payment adjustments support the efforts to make meaningful improvements.
- Support coordinated collection of race and ethnicity data across federal agencies to elevate understanding of health care needs in Black and Latino Americans, Native Americans and other communities of color.
- Increase funding for the health equity infrastructure in the Department of Health and Human Services, including the National Institute on Minority Health and Health Disparities, to better research and address the needs of communities of color.
- Support efforts to increase diversity in the health care workforce, including through federal grants to minority-serving institutions for scholarships.
- Repeal the June 2020 final rule that narrowed the scope of non-discrimination protections under Section 1557 of the Affordable Care Act.
Affordability Resources
Real Affordability Solutions from the Front Lines of Caring
Partnerships, Mergers, and Acquisitions Can Provide Benefits to Certain Hospitals and Communities
Financial Effects of COVID-19: Hospital Outlook for the Remainder of 2021
Results from 2018 Tax-Exempt Hospitals’ Schedule H Community Benefit Reports
Perspective: Confronting Commercial Insurers’ Practices that Threaten Patient Care
Lown Institute Report on Hospital Community Benefits Falls Short
Study: Health insurance market becoming more concentrated
Report: American Medical Association Report on Competition in the Health Insurance