AHA Testimony for the Committee on Ways and Means Subcommittee on Oversight
Testimony
of the
American Hospital Association
for the
Committee on Ways and Means
Subcommittee on Oversight
Of the
U.S. House of Representatives
“Tax-Exempt Hospitals and the Community Benefit Standard”
April 26, 2023
Chairman Schweikert, Ranking Member Pascrell and members of the Subcommittee, I am Melinda Hatton, general counsel and secretary for the American Hospital Association (AHA). On behalf of the AHA’s nearly 5,000 member hospitals, health systems and other health care organizations, our clinician partners — including more than 270,000 affiliated physicians, 2 million nurses and other caregivers — and the 43,000 health care leaders who belong to our professional membership groups, thank you for the opportunity to testify at today’s hearing on tax-exempt hospitals and the community benefit standard.
Every hospital and health system across the nation provides valuable and vital services to the patients and communities they serve. Those include a range of services from urgent to highly specialized care delivered in inpatient settings to many programs and services delivered in the community that advance health and wellness. For example, hospitals and health systems provide financial assistance to help those in need, subsidies for services that would otherwise be unavailable, such as burn or neonatal units, transportation, food pantries, training for the next generation of caregivers and vital research to aid in the treatment of longstanding diseases, such as cancer, and new challenges such as COVID-19. In sum, hospitals do more than any other sector of health care to promote and protect the health of their communities.
Tax-exempt hospitals have special obligations to their communities in exchange for that privilege. They report the amounts they spend on community benefits yearly and conduct a community needs assessment at least every three years. There is no doubt that these hospitals both meet and exceed any requirements and expectations that attach to the privilege of tax exemption. The essential facts are:
- For the most recent tax year for which comprehensive information is available (2019), tax-exempt hospitals devoted nearly 14% of their total expenses to community benefit programs, about half of which was for financial assistance and certain other means tested community benefits.
- The most recent report by the international accounting firm EY demonstrated that the return to taxpayers for hospitals’ federal tax exemption is $9-to-$1; that is for every one dollar of tax exemption taxpayers receive $9 of community benefits. That is a remarkable return by any standard.
A Long History of Community Benefit Beyond Financial Assistance
For the past nearly 100 years, it has been widely recognized that fulfilling a hospital’s charitable mission is multifaceted and does not rest on the provision of financial assistance alone. A sampling of decades of court rulings provides clear evidence for that proposition.
In 1925, the Kansas Supreme Court, in Third Order of St. Dominic v. Younkin, stated unequivocally that hospitals’ charitable obligations went beyond financial assistance:
“When an institution is incorporated for benevolent purposes without capital stock, and no dividends are declared or paid, and conducts a hospital, and all the earnings of the hospital from pay patients, gifts, bequests or whatever sources are used in the maintenance, extension and improvement of the hospital, and which admits patients without regard to race, creed or wealth, it is uniformly held that such hospital is conducted exclusively for charitable purposes.”
Fifteen years later, the Texas Supreme Court built on the Kansas court’s decision in Santa Rosa Infirmary v. City of San Antonio stating:
“[T]he mere fact that pay patients largely predominate over the charity patients, or that the institution did not go into the highways and byways seeking out those to whom its charitable office might be extended, could not, under the great weight of authority, be said to so detract from its charities as to disqualify it as an institution of purely public charity.”
Twenty five years later, in City of Richmond v. Richmond Memorial Hospital, the Virginia Supreme Court went further identifying a greater range of activities that contribute to a hospital’s charitable mission and underscoring that financial assistance was not the touchstone for determining whether a hospital met its charitable obligations:1
“[n]on-profit hospitals which are devoted to the care of the sick, which aid in maintaining public health, and contribute to the advancement of medical science, are and should be regarded as charities. . . .
A tax exemption cannot depend on any such vague and illusory concept as the percentage of free service actually rendered. This would produce chaotic uncertainty and infinite confusion, permitting a hodgepodge of views on the subject.” (emphasis supplied)
Researchers too have recognized that the benefits tax-exempt hospitals provide go beyond financial assistance, including that tax-exempt hospitals are “considerably more likely” to provide unprofitable services, including psychiatric and hospice services.2 The authors of that study warn that overlooking the significance of ownership for service provision “has critical health and spending consequences.”
Through a series of decisions spanning almost a century, the courts and many commentators recognized that hospitals’ charitable mission goes beyond financial assistance.3 In 1969, IRS Revenue Ruling 69-545 memorialized that position and established the “community benefit” standard, which remains in effect today. That ruling and its progeny establish that “promotion of health in a manner beneficial to the community and free of any private benefits or profits is a charitable purpose.” The standard permits hospitals to satisfy their community benefit obligations by providing a mix of financial assistance, services and programs tailored to meet the needs of their communities.
One of greatest accomplishments of the community benefit standard is the flexibility it gives to hospitals and health systems to meet the needs of their communities. A small rural community in Montana will not have the same needs for support and services as a hospital in downtown Atlanta. And it always should be up to those communities to decide if the amount, range and focus of their hospital’s community benefit activities meets their needs. Any suggestion that the IRS should both define and evaluate community benefit clearly misses the point. Community benefit can only be fairly judged by those in the community in which the benefits accrue.
The examples of community benefit activities described in the appendix to this testimony demonstrate that hospitals’ community benefit activities are responsive to their distinctive communities. The following two examples vividly illustrate the benefits of that flexibility:
- HonorHealth in Scottsdale, Ariz., supports the communities it serves through a variety of programs that increase access to health care, provide early childhood education, food bank access, senior day care, and trauma and deployment training for the military professionals. A few examples of the programs and services it provides include distributing 15,000 food boxes to families in need in 2021 through Desert Health. It has an affiliation with a local federally qualified health center to provide more comprehensive care to those in need, including dental and behavioral care, health and nutrition education, and other community resources. It also has a special Military Partnership Program to provide professional educational training to members of the military in areas such as readiness skill sustaining training, medical simulation and nurse transition.
- St. Joseph’s Health in Paterson, N.J., works with a wide range of community partners, including faith-based groups, civic and social organizations, schools and universities, as well as professional groups to offer a wide range of health information and services. Some examples of its commitment to the community it serves include educational programs on autism, diabetes, obesity, asthma and the dangers of substance abuse provided through St. Joseph’s Children’s Hospital. It also provides educational programs and support services for parents of infants and toddlers from birth through age three, with a special focus on children with developmental delays and disabilities. Through its Diabetes Education Center at St. Joseph’s Wayne Medical Center nurse educators provide monthly education and support groups for people with diabetes.
Community Benefit Reporting
In 2008, as part of a major overhaul of Form 990, the IRS developed Schedule H, which is a form for reporting the range of community benefits tax-exempt hospitals provide. The form inquires about a number of areas that pertain to tax-exempt obligations in addition to charts for reporting community benefits at cost. Those include financial assistance, Medicaid underpayments and those from other means-tested programs along with community health improvement services, health professions education, subsidized health services, research, community building, bad debt (attributable to those who would have qualified for financial assistance) and Medicare underpayments. All of those areas pertain directly to a hospital’s community benefit activities and obligations. While the form does not encompass the entire range of care, services, goods and beneficial activities hospitals provide to their communities in service of their health and wellness, it is a good start and hospitals can provide more detail in Schedule O. Schedule O implicitly recognizes that “ease of measurement does not make uncompensated care costs more valuable, financially or otherwise, than providing a mix of services that is less driven by relative profitability.”4
The AHA has been collecting comprehensive information on the benefits reported in Schedule H since 2009.5 Since then, the amount of community benefit has remained steady at roughly 11%-14% of total hospital expenses with financial assistance and Medicaid underpayments counting for about half or more of the total.
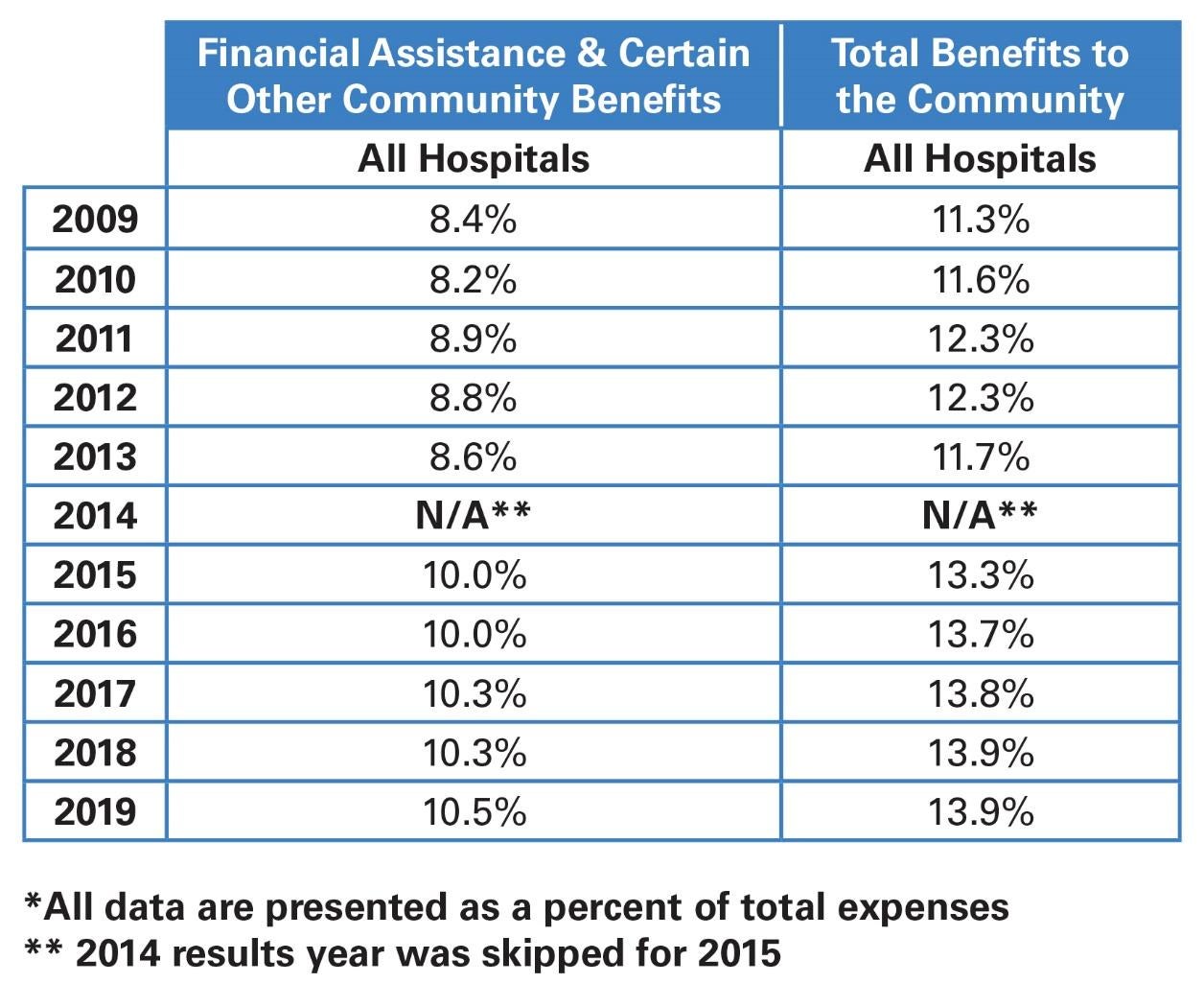
In total, since reporting began hospitals and health systems have provided between $894 billion and $1.3 trillion worth of community benefit, demonstrating an outstanding commitment to their communities. AHA’s annual Schedule H report contains a more detailed breakdown for the total by size, location, type and system-affiliation along with an explanation for the bad debt and Medicare underpayment categories. Both the latter categories represent benefits to patients who needed assistance and gaps filled due to pervasive underpayments.
Community Benefit — Will It Be Affected by the Pandemic?
The suggestion that community benefit declined during the pandemic is premature speculation because no comprehensive data is yet available for tax year 2020. Either the forms have not yet been filed because the IRS allowed more time for filing or they have not been processed by the IRS.
First, it’s important to recognize that there may be no better example of the benefits hospitals provide to their communities than the role they played during the COVID-19 pandemic. Many hospitals collaborated extensively with local public health authorities to implement COVID-19 mitigation strategies, and those effects were felt far beyond the four walls of any hospital. In addition, hospitals and health systems developed public awareness campaigns, and later in the pandemic, served as vaccination sites, working with their staffs and other resources to stand up a rapid vaccination effort to curb the spread of new cases. This activity is a reflection of the energy, commitment and dedication of hospitals’ teams, which may never be fully accounted for on a balance sheet or cost report but should be acknowledged nonetheless.
However, there are a number of factors that could impact the amount and distribution of community benefit during this unprecedented period. First, many hospitals implemented changes to the financial assistance policies to make them more generous.6 However, the impact of those changes could be offset by the dramatic drop in hospital inpatient and outpatient volume in 2020 and continued instability in 2021. Many states restricted hospital volume or capacity in 2020 and 2021. For example, hospitals and health systems in Arizona were limited to 80% occupancy and at least 10 other states imposed a similar policy, reserving between 20%-30% of licensed or intensive care unit ICU beds in case of another COVID-19 surge.
Another factor that could affect the amount and distribution of financial assistance is health insurance coverage gains during the pandemic. The national uninsurance rate reached an “all-time low” of 8% in the first quarter of 2022 due in significant part to increased marketplace premium subsidies and maintenance of effort requirements on state Medicaid programs boosted.
Meanwhile, another factor is that during the pandemic Medicaid and the Children’s Health Insurance Program (CHIP) enrollment grew significantly at the same time more than 39 states made temporary changes to boost Medicaid payment rates. Medicaid and CHIP enrollment grew by 23.3 million enrollees; nearly two-thirds of that increase is among low-income adults (63%) and nearly one-third is among children.7 Combined with volume declines, those temporary expedients presage a dip in Medicaid underpayments. However, as the public health emergency ends, some estimates say 15-18 million people could lose Medicaid coverage, likely boosting the demand for financial assistance and Medicaid underpayments in subsequent years.
Conclusion
The benefits hospitals and health systems provide to their communities far surpass any other sector of health care. Tax-exempt hospitals provide a wide range of benefits most of which are publicly reported each year. Much of the benefits can be tallied from those filings and every year since reporting began they have exceeded the benefit conferred by their federal tax exemption. More importantly, both the numbers and the range of benefits — from financial assistance for care, to backstopping federal programs that consistently underpay, to training and research, community support and the thousands of other efforts hospitals make to promote and protect the health and wellbeing of the communities — demonstrate hospitals’ commitment to their communities and their enduring value.
Appendix 1.
Sampling of Community Benefit Examples – April 2023
UCHealth (Denver, Colo.)
The At-Risk Intervention and Mentoring Program (AIM) at UCHealth University of Colorado Hospital, is a hospital-based violence intervention program that addresses violence as a health issue, aiming to reduce upstream risk factors while enhancing protective factors. AIM specifically identifies youth and adults in the Denver metro area who are at risk of repeat violent injury and links them with hospital and community-based resources that tackle underlying risk factors for violence. The AIM program — an expansion of the program at Denver Health — utilizes best practices, trauma-informed care and a public health approach to provide care. It relies on culturally competent and highly trained outreach workers, paired with public data and research, to interrupt the cycle of violence within these communities. These outreach workers offer support in myriad ways. They meet with patients and their families when they are admitted to the hospital after sustaining an intentional violent injury. They build trusting relationships through culturally sensitive, trauma-informed care. And workers continue to follow patients and families long term to ensure they are connected with support to aid in their healing and recovery process. The list of services they provide ranges from mental health and substance use to legal support, job training and much more. Part of a national effort called The Alliance for Violence Intervention, which builds and connects violence intervention programs and promotes equity for victims of violence globally, AIM is run in partnership with the Gang Rescue and Support Project (GRSP). GRSP is a peer-run, intervention program that works with youth who are at-risk of gang involvement or are presently active in gangs, helps families of gang victims and serves as a youth advocate.
Samaritan Health Services (Corvallis, Ore.)
Responding to community needs is essential to Samaritan Health Services’ mission of “Building Healthier Communities Together.” To that end, the health system collaborates with other local nonprofit organizations to serve people who need health care, regardless of their circumstances and ability to pay, and to help meet other social determinants of health. These efforts are backed up by Samaritan’s vast investment in community health. In 2022, the health system invested more than $174 million in a wide range of community health improvement activities, including programs and workshops attended by more than 28,000 people, health-related research with 915 participants, training for 1,448 health professionals, and grants to local nonprofits in support of health initiatives. Community benefit services include veterans support, chaplain services and maternity care coordination, to name a few. One example of Samaritan Health Services’ investment in its community is its partnership with Pathfinder Clubhouse in Corvallis. This organization provides low-barrier, nonclinical support and other resources to improve the lives of adults living with mental illness. Visit www.samhealth.org/CommunityBenefit for more information.
UMass Memorial Health (Worcester, Mass.)
In 2021, UMass contributed $268.1 million to positively impact the health and well-being of the communities it serves. These community benefit contributions include charity care, subsidized health services, education of health care professionals, research, community-based programming and partnerships. In addition, $85.8 million was absorbed through bad-debt write-offs and Medicare shortfalls. The health system adopted a systemwide anchor mission to address social determinants of health in economically challenged neighborhoods. This initiative is engaged in housing and neighborhood revitalization projects. For example, in 2021 Worcester Common Ground completed a 31-unit housing project to low-income residents. The building features a large community room and a rooftop greenhouse where tenants can grow vegetables in partnership with a youth agriculture program – UMass Memorial invested in this community health improvement effort to address housing and food insecurity. UMass Memorial Health has a strong partnership with UMass Chan Medical School the state’s first and only public academic health sciences center along with the Center for Clinical and Translational Science. It works to educate physicians, scientists and advanced practice nurses to advance health and well-being through pioneering advances in education, research and health care delivery. In addition to participating in cutting-edge research, the health system’s physicians, staff and students commit countless hours to public service efforts to make the region a healthier place to live by harnessing the skills and expertise of the organization to address pressing local needs, such as yearly free flu vaccinations clinics for elderly and other vulnerable populations.
Wellstar Kennestone Hospital (Marietta, Ga.)
Just as health care can extend beyond the doctor’s office, learning can extend beyond the schoolroom. Wellstar Kennestone Hospital and its affiliated OB/GYN and pediatrics offices, recently implemented the Talk With My Baby program in an effort ensure that all babies and toddlers gain the foundational skills necessary to build literacy. Supported by a grant from the Joseph B. Whitehead Foundation, the goal of the program is to ensure that every child can read by third grade. Eighty-five percent of brain growth occurs during the first three years of life, and much of that can be encouraged with regular verbal interaction. The program will educate and support new parents in their important role as their child’s first teachers. Books, of course, are an important resource, but songs, eye contact and just chatting with a young child are all vital parts of building strong language centers in the brain early on. This effort is focused on creating a connected ecosystem with schools and early childhood educators to enhance literacy and create a national model that can be expanded to serve and support our country’s youth. Georgia ranks 41st out of 50 states for literacy, and literacy rates are closely tied to race, ethnicity and ZIP code. This program aims to remove those barriers to equity and equip parents with the tools and knowledge they need so that they, in turn, can support their children. Working with patients and the community, the Talk With My Baby program will help build strong scholars before the school years have even begun.
Meritus Health (Hagerstown, Md.)
Meritus contributed more than $57 million in benefits to the community in fiscal year 2022. The majority of that community benefit was provided through mission-driven health care services, the crucial and foundational support the health system provides to advance health and well-being in the community. Access to health services for all remains a priority with more than $10 million reported for charity care, the free or discounted health and health-related services provided for patients who cannot afford to pay their medical bills. Meritus Health believes that health care is not just for people when they are sick or injured. When obesity was determined to be a top ranked health priority in Washington County, Meritus Health collaborated with the local public health department to create “Healthy Washington County” a coalition of public and private organizations whose mission is to strengthen the health and wellness of our community and residents. Meritus is working to “Go For Bold” and support the community to lose 1 million pounds by 2030. The health system also is investing in the health of the community through the proposed Meritus School of Osteopathic Medicine to ensure that access to care in the community continues for generations to come, providing community-based medical education and by supporting the education of well-trained and socially responsible physicians.
Baystate Health (Springfield, Mass.)
In 2021, Baystate Health hospitals provided over $153 million community benefit including research and educational programs. Research discoveries can translate into better patient care — now and in the future. Baystate researchers conduct clinical, translational and health services research in many medical and surgical specialties and also participate in national clinical trials that study potential new treatment methods and contribute to the advancement of science. Baystate has a technology innovation center that works with technology companies — from one-person startups to tech giants — on innovations like remote monitoring technology and e-visits with health care professionals. The Department of Healthcare Delivery & Population Sciences leverages expertise in population health, clinical effectiveness and outcomes research to focus on making health care more effective and efficient. For example, medical students in Baystate's Population-based Urban and Rural Community Health track were embedded in local community service organizations as part of their Population and Community Health Clerkship to focus on priorities identified by the community including, substance use in rural areas, gun violence, the digital divide for Spanish speakers, and food deserts. Students discussed their projects in a virtual presentation to legislators, community members and faculty.
Mon Health Medical Center (Morgantown, W.Va.)
Mon Health has partnered with local community organizations and health care providers to break down barriers and get people back in the workforce, in particular those who are living in shelters or have lost their job due to COVID-19. Called Pathways to Success (P2S), the initiative is designed to empower positive systemic change that improves the health and lives of individuals in the community. The first P2S cohort included individuals who filled roles at the medical center in housekeeping and environmental services, guest and customer services, registration and nutrition and food service. The program — described as a “hand up” not a “handout” — provides education and training, reliable transportation, health care benefits, daily meals, mentorship and more. As a result of the pilot program, individuals have moved out of a shelter and into their own homes, and others are in the process of securing housing because they now have a steady income. Some individuals have been reconnected with family. To sustain the program and work toward long-term success, the program will continue to partner with community referral organizations.
AtlantiCare (Egg Harbor Township, N.J.)
AtlantiCare is starting early in developing the next generation of health care workers. The hospital hosted its inaugural High School Hiring Blitz, interviewing high school seniors who want to start building their careers in health care and enhance their college applications. The goal is to support students who are looking for learning opportunities and financial resources; build relationships with the next generation of health care workers early on. The high school seniors will work at AtlantiCare Regional Medical Center’s hospital campuses and other areas of the health care system. Jobs include full-time and part-time positions with benefits, as well as pool positions.
UK HealthCare (Lexington, Ky.)
UK HealthCare views community partners as “a large part of who we are.” The Healthcare Jumpstart Program is a partnership between the health system, Bluegrass Community & Technical College (BCTC) and school districts in the state to support students interested in a health care career and also to increase interest in the health care field. In addition, the program will establish a workforce pipeline “to fill critical roles” at hospitals and other health care settings. The Healthcare Jumpstart Program offers students an accelerated path to a nursing career by “providing resources and learning opportunities to earn dual credit while in high school so that they can get a head start on their college education,” according to the UK HealthCare announcement. The dual-credit courses are prerequisites for an associate degree in nursing, or ADN. Students who successfully complete the program at BCTC will be eligible for tuition scholarships and guaranteed employment. Program leaders say that Jumpstart students would be able to earn their ADN in less than two years after high school, preparing them to work as a registered nurse. Advanced practice providers from UK HealthCare will teach some of the BCTC courses. By providing young students with the educational and financial resources to pursue a health care career at an accelerated pace, UK HealthCare is reinforcing their commitment to creating a healthier Kentucky on every level.
Banner Health (Phoenix, Az.)
As a retirement destination, Arizona has the fastest growing rate of Alzheimer’s disease in the nation. The state is expected to see an increase of 33% or more in older adults living with Alzheimer’s between 2020 and 2025. Banner Health and the Banner Alzheimer’s Institute are introducing a new standard of care that provides ongoing hope and help for people with Alzheimer’s and their families. One of the health system’s key focus areas is promoting brain health in underserved communities. Some of the latest efforts include:
- In partnership with Dignity Health, Mayo Clinic and advocate organizations such as the Alzheimer’s Association, Banner Health hosted a day of health and wellness activities aimed at addressing critical health conditions in communities of color and other underserved individuals and families. The focus was on promoting brain health, heart health and stopping the spread of COVID-19. African Americans and Hispanics are disproportionately affected by heart disease, various types of dementia, such as Alzheimer’s disease and COVID-19. Education shared at the event underscored how a health, active lifestyle can decrease the risk of dementia by 40%.
- Banner Health collaborated with Arizona State University on new research that more accurately detects early indicators of the Alzheimer’s disease through neuroimaging — generating images of the brain — and ways to more clearly visualize its physiological signs. Advances in neuroimaging and related medical technologies help physicians better understand how Alzheimer’s disease is developed, how it progresses over time and enable data-driven approaches that will lead to effective treatments that will slow down disease progression and prevent or even cure the disease.
- Banner Health supports The City of Phoenix Memory Café Program, which provides persons living with early to moderate dementia a safe place to socialize and participate in activities facilitated by professionals that stimulate and support brain health. Memory Cafes offer opportunities for care partners to engage in supportive conversations with others and learn how best to support their loved ones.
- Southern Methodist Hosp. & Sanatorium v Wilson, 51 Ariz. 424 at 462 (1938) We think the position that the test of a charitable institution is the extent of the free services rendered, is difficult of application and unsound in theory.
- Jill R. Horwitz and Austin Nichols, Hospital Service Offerings Still Differ Substantially by Ownership Type, Health Affairs, March 2022 (Horwitz)
- Robert Bromberg, Tax Planning for Hospitals, 1977.
- Horwitz at 340.
- 2014 was an exception.
- 2022 JAMA study
- Kaiser Family Foundation