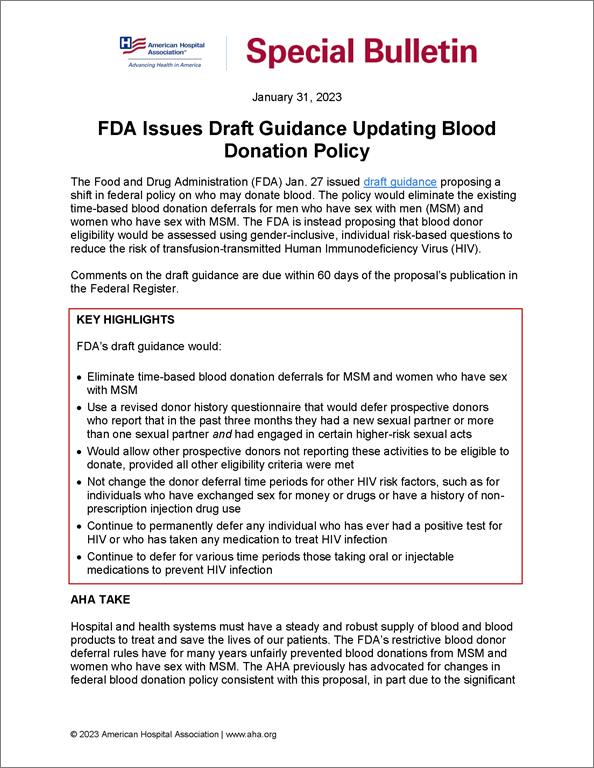
FDA Issues Draft Guidance Updating Blood Donation Policy
AHA Special Bulletin
January 31, 2023
The Food and Drug Administration (FDA) Jan. 27 issued draft guidance proposing a shift in federal policy on who may donate blood. The policy would eliminate the existing time-based blood donation deferrals for men who have sex with men (MSM) and women who have sex with MSM. The FDA is instead proposing that blood donor eligibility would be assessed using gender-inclusive, individual risk-based questions to reduce the risk of transfusion-transmitted Human Immunodeficiency Virus (HIV).
Comments on the draft guidance are due within 60 days of the proposal’s publication in the Federal Register.
Key Highlights
FDA’s draft guidance would:
- Eliminate time-based blood donation deferrals for MSM and women who have sex with MSM
- Use a revised donor history questionnaire that would defer prospective donors who report that in the past three months they had a new sexual partner or more than one sexual partner and had engaged in certain higher-risk sexual acts
- Would allow other prospective donors not reporting these activities to be eligible to donate, provided all other eligibility criteria were met
- Not change the donor deferral time periods for other HIV risk factors, such as for individuals who have exchanged sex for money or drugs or have a history of non-prescription injection drug use
- Continue to permanently defer any individual who has ever had a positive test for HIV or who has taken any medication to treat HIV infection
- Continue to defer for various time periods those taking oral or injectable medications to prevent HIV infection
AHA TAKE
Hospital and health systems must have a steady and robust supply of blood and blood products to treat and save the lives of our patients. The FDA’s restrictive blood donor deferral rules have for many years unfairly prevented blood donations from MSM and women who have sex with MSM. The AHA previously has advocated for changes in federal blood donation policy consistent with this proposal, in part due to the significant strain on the nation’s blood supply in the post-COVID-19 pandemic landscape. For this reason, we are pleased that the new draft guidelines, if finalized, would not only increase the blood supply but correct this historical inequity.
This change in policy would build on the field’s efforts to increase the blood supply, including working with our members and other national health care and blood advocacy groups to urge everyone who can to donate blood.
The AHA will carefully review the draft guidance and submit comments to the FDA.
Highlights of the draft guidance follow.
FDA’S DRAFT GUIDANCE FOR EVALUATING DONOR ELIGIBILITY USING INDIVIDUAL RISK-BASED QUESTIONS
The FDA on Jan. 27 published draft guidance that would eliminate its current three-month deferral period for blood donations from MSM and women having sex with MSM. The agency based its draft policy on a review of available information, including data from other countries with similar HIV epidemiology, including Canada and the United Kingdom, that have instituted this approach, as well as ongoing surveillance of the U.S. blood supply. The FDA indicates that the proposed changes represent an attempt to move toward a gender-inclusive, individual risk-based approach to assessing blood donor eligibility.
The draft guidance would accomplish this by proposing revisions to the donor history questionnaire to include questions for all prospective donors about new or multiple sexual partners in the last three months. Based on the available data, the agency believes the implementation of the proposed individual risk-based questions will not compromise the blood supply’s safety or availability.
Specifically, FDA’s draft guidance would revise its current donor history questionnaire to ask all prospective donors whether they have had a new or multiple sexual partners in the past three months. Prospective donors replying affirmatively to this question would then be asked about their history of anal sex in the previous three months, according to the proposed guidance. It would also defer prospective donors reporting that, within the past three months, they had a new sexual partner or more than one sexual partner and had anal sex.
All other prospective donors could be considered as possibly eligible to donate, provided all other eligibility criteria are met.
Other provisions in the draft guidance remain unchanged from existing FDA policy, including:
- no changes in the donor deferral time periods for other HIV risk factors, including for individuals who have exchanged sex for money or drugs, or have a history of non-prescription injection drug use;
- continuing to permanently defer any individual who has ever had a positive test for HIV or who has taken any medication to treat HIV infection; and
- continuing to require blood establishments to test all blood donations for evidence of certain transfusion-transmitted infections, including HIV, hepatitis B and hepatitis C.
FDA also notes that available data demonstrate that the use of pre-exposure prophylaxis (PrEP) or post-exposure prophylaxis (PEP) may delay detection of HIV in licensed screening tests for blood donations, potentially resulting in false negative results. The agency notes that some blood establishments currently have deferral policies related to the use of such medications to prevent HIV infections. As a result, FDA’s proposed guidance would also defer for three months individuals taking oral medications to prevent HIV infection, such as PrEP or PEP, and defer for two years from their most recent injection individuals taking injectable PrEP to prevent HIV infection.
The FDA notes that although these draft recommendations, when finalized, will potentially increase the number of individuals eligible to donate blood, some individuals will still be deferred from donating blood. Nevertheless, the agency stresses that that individuals taking PrEP should not stop taking these medications in order to potentially be eligible to donate blood. Instead, the FDA says it will continue to track the latest data relevant to PrEP and blood donation and propose future updates to their guidance, as appropriate.
FURTHER QUESTIONS
If you have further questions, contact Roslyne Schulman, AHA’s director of outpatient payment policy, at rschulman@aha.org.