MIPS Alternative Payment Model Participants Reporting under MIPS
Some clinicians who participate in APMs will not qualify for exemption from the Merit-based Incentive Payment System (MIPS), nor the advanced APM payment incentives, either because the APM does not qualify as an advanced APM (such as Track 1 of the Medicare Shared Savings Program (MSSP)), or because the clinician did not meet the participation thresholds to qualify for MIPS exemption. However, some advantages still exist for clinicians subject to MIPS who also participate in certain Medicare APMs.
Specifically, CMS has designated certain Medicare APMs as “MIPS APMs.” In 2017, these include Tracks 1, 2 and 3 of the MSSP and the Next Generation Accountable Care Organization (ACO) program. A full list of APMs that qualify as MIPS APMs is available on CMS’s website. Clinicians who participate in one of these MIPS APMs receive favorable scoring under the MIPS. To identify which clinicians are part of a MIPS APM, at the end of each quarter of the performance period – March 31, June 30, Sept. 30 and Dec. 31 – CMS will review the Participation List each APM entity (the entity that contracts with CMS for financial and quality outcomes – in this case, the ACO) must submit. Clinicians who appear on the Participation List on at least one of those dates would be included in the APM entity for the purposes of MIPS scoring. All individual clinicians and groups in an APM entity will contribute to and share the same composite final score for the purposes of the MIPS.
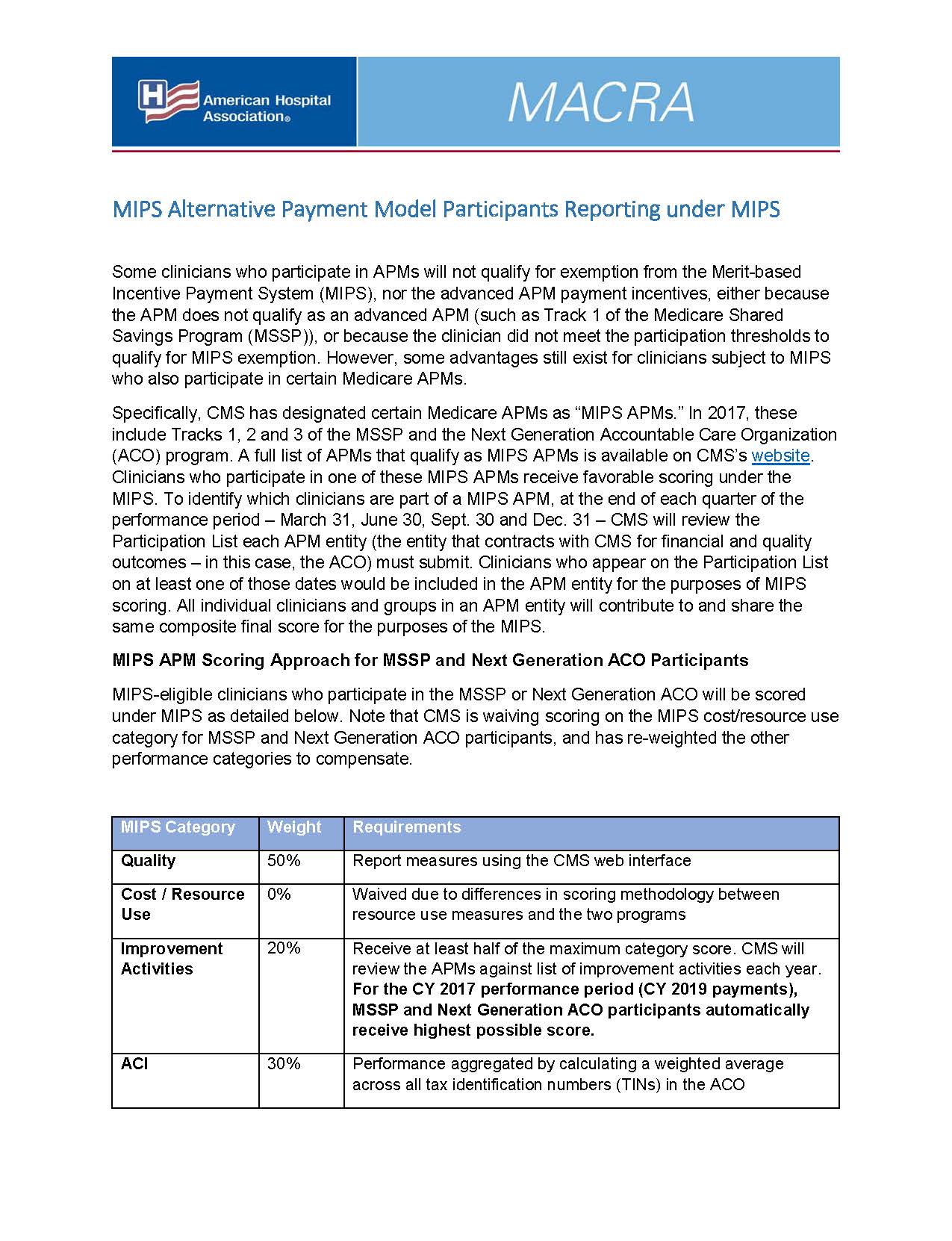
MIPS APM Scoring Approach for MSSP and Next Generation ACO Participants
MIPS-eligible clinicians who participate in the MSSP or Next Generation ACO will be scored under MIPS as detailed below. Note that CMS is waiving scoring on the MIPS cost/resource use category for MSSP and Next Generation ACO participants, and has re-weighted the other performance categories to compensate.
MIPS Category | Weight | Requirements |
Quality | 50% | Report measures using the CMS web interface |
Cost / Resource Use | 0% | Waived due to differences in scoring methodology between resource use measures and the two programs |
Improvement Activities | 20% | Receive at least half of the maximum category score. CMS will review the APMs against list of improvement activities each year. For the CY 2017 performance period (CY 2019 payments), MSSP and Next Generation ACO participants automatically receive highest possible score. |
ACI | 30% | Performance aggregated by calculating a weighted average across all tax identification numbers (TINs) in the ACO |
MIPS Category Weight Requirements Quality 50% Report measures using the CMS web interface Cost / Resource Use 0% Waived due to differences in scoring methodology between resource use measures and the two programs Improvement Activities 20% Receive at least half of the maximum category score. CMS will review the APMs against list of improvement activities each year. For the CY 2017 performance period (CY 2019 payments), MSSP and Next Generation ACO participants automatically receive highest possible score. ACI 30% Performance aggregated by calculating a weighted average across all tax identification numbers (TINs) in the ACO
Scoring for MIPS APMs other than MSSP and Next Generation ACO
For other MIPS APMs, CMS will not score clinicians on either the quality or resource use categories of the MIPS. As a result, 25 percent of the final score will be based on meeting the requirements of the improvement activity category, while the remaining 75 percent will be based on performance in the ACI category. CMS may revise this approach in future years as it gains experience with the models.
Additional details regarding MIPS reporting can be found here.
Download the MIPS Alternative Payment Model Participants Reporting under MIPS PDF below.

