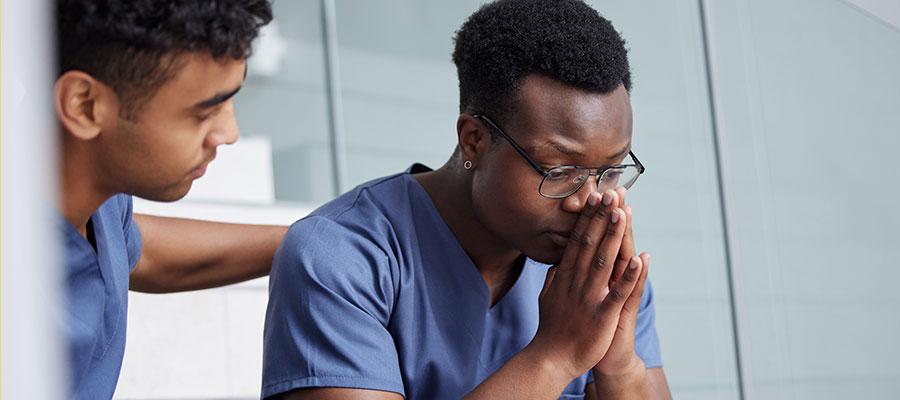
Preventing suicide in the health care workforce depends on all of us
September is National Suicide Prevention Month, with several days that emphasize the opportunity to elevate awareness about the important role everyone can play in suicide prevention and the importance of being there for the people in our lives (#BeThere), especially those who may be struggling or in crisis. September 10 was World Suicide Prevention Day and September 17 is National Physician Suicide Awareness Day.
A recent public poll suggests that mental health has become a leading priority in the U.S., with 76% of people saying their own mental health is equally important to physical health. More than 8 in 10 adults (84%) say that as a result of the pandemic, it's more important than ever to make suicide prevention a national priority. Public sentiment that suicide can and should be prevented is strong, and help is available 24/7 by calling 988, the Suicide and Crisis Lifeline.
However, real or perceived access to quality suicide-specific care is limited for some. When I talk about suicide with health care professionals, I often start by asking for a show of hands: “How many people would bring their loved one who was having thoughts of suicide or needed treatment for suicidality to the health care system in which you work?” Typically, far less than half the hands in the room go up. Given this, it is not surprising that many health care providers frequently bury or ignore their own thoughts of suicide. In addition to perhaps questioning whether effective treatment options exist (they do!), many providers also don’t attend to their own thoughts of suicide out of fear over what their colleagues, supervisors or patients might think or the repercussions that could happen – whether those repercussions are real or just perceived.
Along with individual action, the systems in which health care providers work have a role to play in suicide prevention. It is the responsibility of health care leadership to ensure that they build a restorative and just culture where taking care of oneself is expected, respected and modeled, and where access to quality, effective treatment for suicide is available. The Suicide Prevention in the Health Care Workforce guide, produced by the AHA and the CDC, is a resource that offers hospitals and health systems proven strategies to improve the mental health and well-being of their staff. Evidence-based practices for suicide do exist and, when used with fidelity, health care systems are substantially reducing suicides for patients in their care. Health care systems that have adopted Zero Suicide typically find that the program adds neither labor nor cost; in fact, most systems find it to be a more efficient use of resources. Visit Zero Suicide for more information on best practices for health care systems.
During Suicide Prevention Month, make it a point to check in on your colleagues, friends, patients, as well as yourself. Ask directly when you are concerned about suicide risk (“Are you thinking about killing yourself?”) and provide support (check in regularly with them). Health care leadership should work to eliminate stigma around seeking care; ensure access to quality treatment is available when and how it is needed; and that job stressors are acknowledged and reduced.
Flight attendants tell parents to put on their own oxygen masks before assisting others, even though every parent’s first instinct is to protect their child over themselves. Health care workers share this propensity, which can make them invaluable caregivers – but also vulnerable to ignoring their own health and well-being. Know that your strength and capacity as a health care provider grows stronger when you put your oxygen mask on first. Please do this for yourself and encourage others to do the same.
Julie Goldstein Grumet
Vice President, Suicide Prevention Strategy
Director, Zero Suicide Institute
Education Development Center
Learn more about suicide prevention in the health care workforce.

