Fact Sheet: Hospital Price Transparency
August 2025
The Issue
Hospitals and health systems are committed to empowering patients with the information they need to live their healthiest lives. This includes ensuring they have access to accurate price information when seeking care. Most hospitals use cost estimate tools to provide patient-specific price information because every course of care is unique.
Hospitals and health systems are working to comply with both state and federal price transparency policies, which include the federal Hospital Price Transparency requirements and provisions in the No Surprises Act. The Centers for Medicare & Medicaid Services (CMS) monitors hospital price transparency compliance, which includes requirements for a consumer-friendly display of shoppable services information, as well as comprehensive, machine-readable files. Since the Hospital Price Transparency requirements went into effect in 2021, hospitals have invested countless staff hours and substantial resources in adhering to the provisions and remain committed to ensuring they meet the regulatory requirements, even as they have been continually modified since implementation.
AHA Position
The AHA supports price transparency efforts that help patients access clear, accurate information about prices when preparing for hospital care, as well as ensuring employers have the needed information as the primary purchasers of health care through employer-sponsored insurance. The AHA also supports aligning federal price transparency requirements to avoid confusion and duplication of effort that adds unnecessary cost and burden to the health care system.
Key Facts
Hospitals and health systems are subject to several different federal price transparency policies, often in addition to similar policies at the state level. These include:
- Hospital Price Transparency Rule. As of Jan. 1, 2021, hospitals are required to publicly post, via machine-readable files that include chargemaster data, information on self-pay prices for all services and all negotiated rates with commercial payers. The rule also requires hospitals to provide patients with an out-of-pocket cost estimator tool or payer-specific negotiated rates for at least 300 shoppable services.
- Uninsured/Self-pay Good Faith Estimates. The No Surprises Act requires hospitals and other providers to share good-faith estimates with uninsured/self-pay patients for most scheduled services. Future regulations will require unaffiliated providers to combine their estimates for an uninsured/selfpay patient into a single, comprehensive good-faith estimate for an episode of care.
- Insured Good Faith Estimates and Advanced Explanation of Benefits. The No Surprises Act requires insurers to share with their enrollees advanced explanations of benefits, though implementation is currently on hold pending rulemaking. Hospitals will need to provide good-faith estimates to health insurers to operationalize this policy.
Implementation Considerations
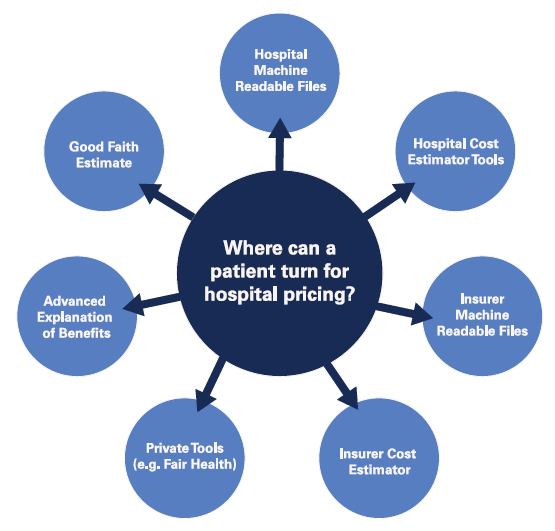 Patients face numerous and potentially conflicting sources of pricing information. The Hospital Price Transparency Rule, the health insurer Transparency in Coverage Rule and the No Surprises Act’s price transparency policies each feature one or more ways in which patients can access pricing information in advance of care. A patient who seeks price information may do so through the following mechanisms: the hospital’s machine-readable files; the hospital’s online patient cost estimator; the health insurer’s machine-readable files; the health insurer’s online cost estimator; the advanced explanation of benefits created by the health plan; or a good-faith estimate created by the provider in the event they want to consider their self-pay options. Separately, state-level policies may direct patients to a variety of other price-estimating options from private sector vendors. Unfortunately, none of these resources has been designed to complement one another, and the information provided to patients is calculated in different ways. As a result, the reported rate information may be inconsistent, and patients do not have a clear indicator as to which source should be relied upon. As a result, the overabundance of tools may create patient confusion rather than provide value.
Patients face numerous and potentially conflicting sources of pricing information. The Hospital Price Transparency Rule, the health insurer Transparency in Coverage Rule and the No Surprises Act’s price transparency policies each feature one or more ways in which patients can access pricing information in advance of care. A patient who seeks price information may do so through the following mechanisms: the hospital’s machine-readable files; the hospital’s online patient cost estimator; the health insurer’s machine-readable files; the health insurer’s online cost estimator; the advanced explanation of benefits created by the health plan; or a good-faith estimate created by the provider in the event they want to consider their self-pay options. Separately, state-level policies may direct patients to a variety of other price-estimating options from private sector vendors. Unfortunately, none of these resources has been designed to complement one another, and the information provided to patients is calculated in different ways. As a result, the reported rate information may be inconsistent, and patients do not have a clear indicator as to which source should be relied upon. As a result, the overabundance of tools may create patient confusion rather than provide value.- Hospitals are working to provide the most accurate estimates for what a patient may need to pay. In response to the growing desire from patients for digital tools to support their health care, many hospitals and health systems have embraced new technologies that enable patients to obtain tailored out-of-pocket cost estimates through online tools.
- Hospitals are working to provide the most accurate estimates for what a patient may need to pay. In response to the growing desire from patients for digital tools to support their health care, many hospitals and health systems have embraced new technologies that enable patients to obtain tailored out-of-pocket cost estimates through online tools.
- While hospitals are working to comply with the requirement to post machine-readable files, the nature of hospital pricing and rate negotiations does not translate easily into a single, fixed rate per service. Hospitals’ contracts with health plans are complex, and the actual rate that may apply to a service (or bundle of services) can vary dramatically based on a patient’s specific scenario (e.g., how many services are delivered during an episode of care or how ill the patient is). In addition, in most instances, the patient will only owe a portion of the final negotiated amount due to their health plan’s cost-sharing rules.
- Price transparency tools require large investments in staff time and hospital resources. Hospitals’ commitment to compliance is led by their desire to provide the most accessible and useful information to patients. This requires extensive investment in personnel and finances. Price transparency tools, including patient-specific cost estimator tools and machine-readable files, require the adoption of new technologies that can pull relevant data from multiple sources and present it to patients in the easiest-to-navigate manner. With respect to the machine-readable files, the resulting output can often be too large to be housed on existing hospital websites, and the data must be refreshed frequently.
- CMS has been working closely with hospitals on compliance. CMS began auditing hospital compliance with the Hospital Price Transparency Rule as early as the spring of 2021, and to date has reviewed thousands of hospitals’ machine-readable files and shoppable service tools. As of May 2025, the agency has only issued twenty-seven fines for non-compliance. Hospitals and health systems report that the agency has worked with them to understand the contractual complexities and navigate the regulatory guidance to identify and resolve any compliance issues.
- Third-party “compliance” reports miss the mark. Some third parties continue to issue reports mischaracterizing whether hospitals are complying with the Hospital Price Transparency Rule. These reports fail to align their compliance assessment with CMS’ requirements. This misrepresentation of the requirements has only served to advance misinformation and confusion on the issue and distract from genuine, productive discussions and efforts around what patients want in terms of transparent data and how best to provide that information.
Recommendations
Hospitals and health systems are eager to continue working towards providing the best possible price estimates for their patients. We ask Congress and the administration to take the following steps to support these efforts, including:
- Review and streamline the existing transparency policies with a priority objective of reducing potential patient confusion and unnecessary regulatory burden on providers.
- Focus efforts on ensuring pre-service estimates are as accurate as possible, including by simplifying benefit design.
- Remove providers from the cost-sharing collection process and instead require insurers to be responsible for cost-sharing estimates and collections.
- Continue to convene patients, providers and payers to seek input on how to make federal price transparency policies as patient-centered as possible.
- Refrain from advancing additional legislation or regulations that may further confuse or complicate providers’ ability to provide meaningful price estimates while adding unnecessary costs to the health care system.