AHA Statement on “Health Care Spending in the United States: Unsustainable for Patients, Employers, and Taxpayers”
Statement
of the
American Hospital Association
for the
Subcommittee on Health
of the
Committee on Energy and Commerce
U.S. House of Representatives
“Health Care Spending in the United States: Unsustainable for Patients, Employers, and Taxpayers”
January 31, 2024
On behalf of our nearly 5,000 member hospitals, health systems and other health care organizations, our clinician partners — including more than 270,000 affiliated physicians, 2 million nurses and other caregivers — and the 43,000 health care leaders who belong to our professional membership groups, the American Hospital Association (AHA) writes to share the hospital field’s comments on the topic of national health expenditures.
OVERVIEW OF NATIONAL HEALTH SPENDING
We welcome the opportunity to provide comments to the subcommittee regarding health care spending. America’s hospitals and health systems — physicians, nurses and other caregivers — understand and share concerns regarding the high cost of health care and are working hard to make care more affordable by transforming the way health care is delivered in our communities. However, government payers continue to pay below the cost of care, and commercial insurers are erecting barriers to payment. Real change will require an effort by everyone involved, including providers, the government, employers and individuals, device makers, drug manufacturers, insurers and other stakeholders.
Commercial Insurer Accountability
To truly reduce health care costs, we urge the subcommittee to address practices by certain commercial health insurers. Additional oversight is needed to ensure that certain Medicare Advantage (MA) plans can no longer engage in tactics that restrict and delay access to care while adding burden and cost to the health care system.
While MA plans were designed to help increase efficiency in the Medicare program, recently released data from the Medicare Payment Advisory Commission (MedPAC) found that MA plans will be responsible for $88 billion in excess federal spending this year, due in part to inappropriate upcoding practices, whereby plans report enrollees as having more health conditions and being sicker than they are to receive higher reimbursements. At the same time, health insurance premiums continue to grow — in fact, annual insurance premiums increased nearly twice as much as hospital prices over a ten-year period.1
Additionally, inappropriate denials for prior authorization and coverage of medically necessary services remain a pervasive problem among certain MA plans. A report from the Department of Health and Human Services (HHS) Office of Inspector General in 2022 found that MA plans are denying at a high rate medically necessary care that met Medicare criteria.2 The report highlights that 13% of prior authorization denials and 18% of payment denials met Medicare coverage rules and therefore should have been approved. In a program this size — covering more than half of all Medicare beneficiaries — improper denials at this rate are unacceptable. However, because the government pays MA plans a risk-adjusted per-beneficiary capitation rate, there is a perverse incentive to deny services to patients or payments to providers to boost profits.
These practices delay access to care for seniors and add financial burden and strain on the health care system through inappropriate payment denials and increased staffing and technology costs to comply with plan requirements. They are also a major burden to the health care workforce and contribute to provider burnout.
We urge the subcommittee to pass legislation to build on these regulations with further oversight of the MA program, including greater data collection and reporting on plan performance and more streamlined pathways to report suspected violations of federal rules.
Prescription Drug Prices
The subcommittee should also address the high costs of prescription medications, given the regular increases in costs, as this impacts expenses for all providers, including hospitals. For instance, a recent report noted pharmaceutical companies raised list prices on 775 brand name drugs during the first half of January 2024, with a median increase of 4.5%, though the prices of some drugs rose by 10% or higher.3 These increases were higher than the rate of inflation, which was 3.4% in December.
A report by the Assistant Secretary for Planning & Evaluation at HHS found that drug companies increased drug prices for 1,216 drugs — many used to treat chronic conditions like cancer and rheumatoid arthritis — by more than the rate of inflation, which was 8.5% between 2021 and 2022.4 In fact, the average price increase for these drugs was 31.6%, with some drugs experiencing price increases as much as 500%. Moreover, recent drug shortages, specifically for certain drugs used to treat cancer, have also fueled further expense growth. It is estimated that drug shortages alone cost hospitals nearly $360 million a year.5
SITE-NEUTRAL PAYMENT POLICIES
The AHA strongly opposes efforts to expand site-neutral payment cuts. Current Medicare payment rates appropriately recognize that there are fundamental differences between patient care delivered in hospital outpatient departments (HOPDs) compared to other settings. HOPDs provide important access to care for Medicare beneficiaries, many of which are more likely to be sicker and more medically complex than those treated at physicians’ offices, while also being held to stricter safety and regulatory requirements.
This is especially true in rural communities. Medicare beneficiaries in rural areas — including those who are dually eligible for Medicaid — disproportionately rely on HOPDs to meet their increased health care needs since they have less access to office-based physicians.6 Additional Medicare cuts to these facilities will have a direct impact on the level of care and services available to vulnerable patients in rural communities.
The AHA opposes provisions in H.R. 5378, the Lower Costs, More Transparency Act (LCMTA), to expand site-neutral payment cuts to include essential drug administration services furnished in off-campus HOPDs. This policy disregards important differences in patient safety and quality standards required in these facilities. Unlike other sites of care, hospitals take additional steps to make certain that drugs are prepared and administered in a safe manner for both patients and providers.7 For example, hospital pharmacists are available on-site to confirm safe dosing and check for drug interactions. Hospitals also provide patients with rapid access to comprehensive wraparound services and multidisciplinary care coordination. In addition, hospitals must adhere to multiagency federal and state regulatory standards to ensure safety oversight, including those required by the Food and Drug Administration, U.S. Pharmacopeia and The Joint Commission.
The cost of care delivered in hospitals and health systems considers the unique benefits they provide to their communities, and which are not provided by other sites of care. This includes investments made to maintain standby capacity for natural and manmade disasters, public health emergencies and unexpected traumatic events, as well as delivering 24/7 emergency care to all who come to the hospital.
Existing site-neutral payment cuts have already created significant financial challenges for many hospitals and health systems. This is largely because Medicare underpays hospitals for the cost of caring for patients. The latest analysis shows that on average Medicare pays only 82 cents for every dollar of hospital care provided to Medicare beneficiaries, leaving hospitals with nearly $100 billion in Medicare shortfalls in 2022 alone.8 As a result, two-thirds of all hospitals reported negative Medicare margins in 2022.
Any additional site-neutral cuts would exacerbate these financial challenges and reduce access to essential care and services in communities, especially those in rural and underserved areas.
Separate Unique Health Identifier
The AHA opposes the provision in the LCMTA that would require each off-campus HOPD to be assigned a separate unique health identifier from its provider. This is unnecessary since hospitals are already transparent about the location of care delivery on their bills. Hospitals and other providers bill according to federal regulations, which require them to bill all payers — Medicare, Medicaid and private payers — using codes that indicate the location of where a service is provided. As a result, this provision would impose an unnecessary and onerous administrative burden on providers and needlessly increase Medicare program administrative costs.
This provision also would require that as a condition of payment, hospitals submit an attestation of compliance with the Medicare provider-based regulations for each of their off-campus HOPDs within two years of enactment. Given hospitals’ experience with review and approval of similar attestations in the past, we are concerned that this requirement would be extremely burdensome for hospitals and Medicare contractors.
PRICE TRANSPARENCY REQUIREMENTS
We appreciate the subcommittee’s ongoing interest in hospital price transparency to provide consumers with the price information they need specific to their course of treatment. However, in seeking to codify the Hospital Price Transparency Rule that went into effect in January 2021, the provisions of LCMTA undermine the work hospitals have done to provide price information to consumers and are redundant to recent actions taken by CMS.
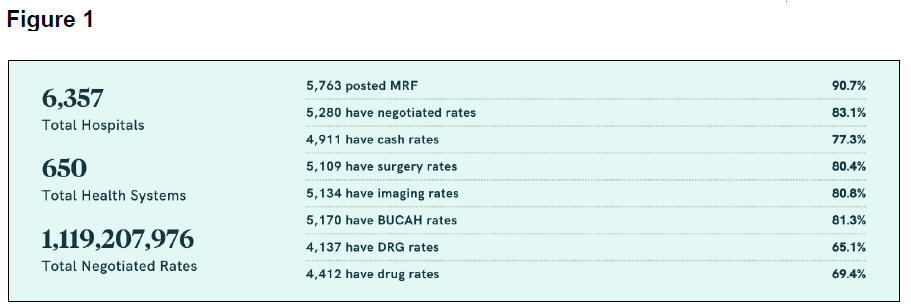
Hospitals and health systems have invested considerable time and resources to comply with the conditions of the Hospital Price Transparency Rule, which requires online access to both a machine-readable file and a list of shoppable services. Recent data from Turquoise Health shows that 90.7% of hospitals have met the requirement to post a machine-readable file, and 83.1% have included a substantial amount of negotiated rates (see Figure 1).9
One of the most significant changes from the current rule would be that the LCMTA no longer recognizes price estimator tools as a method to meet the shoppable services requirement. This change would both reduce access to a consumer-friendly research tool and unfairly penalize hospitals that have spent significant capital to comply with the regulation. These facilities would instead need to develop and maintain a shoppable services spreadsheet, which may be difficult for consumers to navigate and will not reflect the different policies that their insurer may apply to determine the final price for a service. Price estimator tools offer consumers an estimate of their out-of-pocket costs based on their insurance benefit design, such as cost-sharing requirements and prior utilization, as well as the patient’s annual deductible. This is a very important feature of these tools that is not available from a shoppable services spreadsheet. Eliminating the use of price estimator tools as a method to meet the shoppable services requirement of the Hospital Price Transparency Rule would therefore reduce price transparency for patients. We urge Congress to reject this change to hospital transparency requirements.
CONCLUSION
Thank you for your consideration of the AHA’s comments on issues related to health care expenditures. We look forward to continuing to work with you to address these important topics on behalf of our patients and communities.
__________
1 https://www.aha.org/system/files/media/file/2022/04/2022-Hospital-Expenses-Increase-Report-Final-Final.pdf
2 https://oig.hhs.gov/oei/reports/OEI-09-18-00260.pdf
3 https://www.wsj.com/health/pharma/drugmakers-raise-prices-of-ozempic-mounjaro-and-hundreds-of-other-drugs-bdac7051
4 https://aspe.hhs.gov/reports/prescription-drug-price-increases
5 https://www.axios.com/2023/03/21/drug-shortages-upend-cancer-treatments
6 https://www.aha.org/system/files/media/file/2024/01/analysis-hospitals-health-systems-are-critical-to-preserving-access-to-care-for-rural-communities-report.pdf
7 https://www.aha.org/system/files/media/file/2023/11/Reject-Site-Neutral-Payment-for-Lower-Standards-of-Infusion-Care.pdf
8 https://www.aha.org/system/files/media/file/2024/01/medicare-significantly-underpays-hospitals-for-cost-of-patient-care-infographic.pdf
9 https://blog.turquoise.health/moving-into-2024-state-of-price-transparency/

