Adjusting Payment Under MIPS
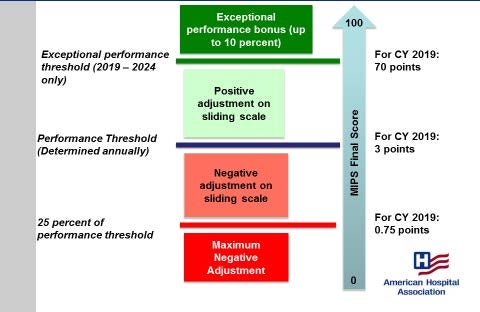
To translate clinicians’ MIPS final performance scores into payment adjustments, CMS will identify several final score thresholds.
- A performance threshold. Clinicians who score above the performance threshold will receive positive payment adjustments on a sliding scale, and clinicians who score below the threshold will receive negative payment adjustments on a sliding scale. CMS will publish the performance threshold prior to the start of each performance period so that MIPS participants know what level of performance is expected in order to receive positive or negative adjustments.
For calendar year (CY) 2017 (affecting CY 2019 MIPS payment), the performance threshold is three points. This threshold aligns with CMS’s “Pick Your Pace” approach in which reporting any one measure, one improvement activity or meeting all base advancing care information (ACI) category requirements results in three points. - 25 percent of the performance threshold. At or below this score, MIPS-eligible clinicians and groups receive the maximum negative payment adjustment (-4 percent in CY 2019). For CY 2017 (affecting CY 2019 MIPS payment), this value is 0.75 points. CMS has stated that it is highly unlikely that any clinician or group would receive a score of 0.75 points for 2017 – instead, they would receive at least three points for reporting some data, or zero points for reporting no data at all.
- An exceptional performance threshold. At or above this score, MIPS-eligible clinicians and groups are eligible for an additional bonus beyond their positive MIPS adjustment. For CY 2017 (affecting CY 2019 MIPS payment), this value is 70 points. Therefore, all clinicians and groups receiving a score at or above 70 would be eligible for exceptional performance bonuses. CMS will pay out $500 million in exceptional performance bonuses in CYs 2019 through 2024.
Figure 1: Translating MIPS Performance Scores into Payment Adjustments
Scaling Factor for Positive Payment Adjustments
As required by the MACRA, CMS must implement MIPS payment adjustments in a budget- neutral manner. That is, the agency may not pay out more in incentive payments than it recoups in penalties.
The MACRA enables CMS to apply a scaling factor of up to 3.0 to positive payment adjustments to maintain the budget neutrality of the MIPS. The scaling factor likely will be applied in years where CMS is taking in a significant amount in MIPS performance penalties. In CY 2019, this means that clinicians and groups could receive positive payment adjustments as high as 12 percent. However, CMS believes it is unlikely that the agency would need to apply the full scaling factor.

