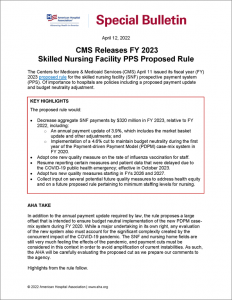
CMS Releases FY 2023 Skilled Nursing Facility PPS Proposed Rule
Special Bulletin
April 12, 2022
The Centers for Medicare & Medicaid Services (CMS) April 11 issued its fiscal year (FY) 2023 proposed rule for the skilled nursing facility (SNF) prospective payment system (PPS). Of importance to hospitals are policies including a proposed payment update and budget neutrality adjustment.
Key Highlights
The proposed rule would:
- Decrease aggregate SNF payments by $320 million in FY 2023, relative to FY 2022, including:
- An annual payment update of 3.9%, which includes the market basket update and other adjustments; and
- Implementation of a 4.6% cut to maintain budget neutrality during the first year of the Payment-driven Payment Model (PDPM) case-mix system in FY 2020.
- Adopt one new quality measure on the rate of influenza vaccination for staff.
- Resume reporting certain measures and patient data that were delayed due to the COVID-19 public health emergency; effective in October 2023.
- Adopt two new quality measures starting in FYs 2026 and 2027.
- Collect input on several potential future quality measures to address health equity and on a future proposed rule pertaining to minimum staffing levels for nursing.
AHA TAKE
In addition to the annual payment update required by law, the rule proposes a large offset that is intended to ensure budget neutral implementation of the new PDPM case-mix system during FY 2020. While a major undertaking in its own right, any evaluation of the new system also must account for the significant complexity created by the concurrent impact of the COVID-19 pandemic. The SNF and nursing home fields are still very much feeling the effects of the pandemic, and payment cuts must be considered in this context in order to avoid amplification of current instabilities. As such, the AHA will be carefully evaluating the proposed cut as we prepare our comments to the agency.
Highlights from the rule follow.
PROPOSED SNF PPS PAYMENT CHANGES
The aggregate impact of this proposed rule would be a cut of $320 million to the SNF PPS in FY 2023, relative to FY 2022 levels. This takes into account both the annual payment update and the one-time budget neutrality offset for the first year of PDPM implementation.
Proposed FY 2023 Payment Update
The rule’s proposed annual update would increase net payments to SNFs by 3.9% in FY 2023 relative to FY 2022. This includes a 2.8% market-basket update offset by a statutorily-mandated cut of 0.4 percentage point for productivity. The update also includes a 1.5 percentage point increase to counter the agency’s market basket error in FY 2021. The forecast error was determined by comparing the projected versus actual market basket that year, 1.5 percentage point, exceeding the 0.5 percentage point threshold required to trigger a correction.
Proposed PDPM Offset
The rule discusses CMS’ ongoing effort to determine whether implementation of the PDPM in FY 2020 was executed in a budget-neutral manner, meaning that aggregate payments were equal to what total payments would have been under the prior system. Based on the agency’s finding that FY 2020 payments were higher under PDPM than they would have been under the prior system, the rule proposes to apply a negative 4.6% PDPM “parity adjustment,” for a total cut of $1.7 billion in FY 2023. CMS believes that this cut would enable the ongoing budget-neutral implementation of PDPM. In addition, the agency specifically did not propose a phase-in of this cut in order to avoid the “continuing accumulation of excess SNF payments, which we cannot recoup.”
The rule also describes the steps taken by CMS to isolate the impact of the market basket increase and the COVID-19 public health emergency in FY 2020 from its assessment of budget neutrality. Specifically, CMS’ analysis found an increase in Medicare Part A SNF spending, even after accounting for these effects, and shares analyses indicating that the public health emergency (PHE) had only a marginal impact on SNF/nursing home operations. However, these findings are in stark contrast with the experience of many providers in the field.
SNF QUALITY REPORTING PROGRAM (QRP)
CMS proposes to adopt one new quality measure and revise the compliance date for reporting of certain measures and patient assessment data that was previously delayed due to the COVID-19 PHE.
Proposed Adoption of Influenza Vaccination among Health Care Personnel Measure
CMS proposes to adopt the Centers for Disease Control and Prevention (CDC)-developed Influenza Vaccination Coverage among Healthcare Personnel measure beginning with the FY 2025 SNF QRP. This measure is endorsed by the National Quality Forum and is currently reported in the inpatient rehabilitation facility and long-term care hospital quality reporting programs. It is a process measure that evaluates the percentage of health care personnel who are physically present in the health care facility for at least one working day between Oct. 1 and March 31 of the following year who received an influenza vaccine any time from when it first became available. “Healthcare personnel” is defined as all paid and unpaid persons working in a health care setting, contractual staff not employed by the health care facility, and persons not directly involved in patient care but potentially exposed to infection agents that can be transmitted to and from health care personnel. If finalized, SNFs would submit data for the measure through the CDC’s National Healthcare Safety Network collection and submission framework.
Proposed Revised Compliance Date for Certain Measures and Data Reporting
SNFs were originally scheduled to begin collecting data on two new quality measures, Transfer of Health Information to the Patient and Transfer of Health Information to the Provider, as well as certain standardized patient assessment data elements (SPADEs) beginning Oct. 1, 2020. Given the effects of the COVID-19 PHE, CMS delayed these requirements until Oct. 1 of the year that is at least two full fiscal years after the end of the COVID-19 PHE. However, CMS believes that SNFs are able to fulfill these requirements sooner than this deadline, and thus in this rule proposes to require collection of these data beginning Oct. 1, 2023.
Request for Comment
CMS seeks comment on several topics, including quality measures for use in future years of the SNF QRP. In a distinct request for information (RFI), CMS requests stakeholder feedback on the future adoption and implementation of the CoreQ: Short Stay Discharge Measure into the SNF QRP; this measure calculates the percentage of individuals discharged in a six-month period from a SNF who are satisfied with their SNF stay as reported on the CoreQ questionnaire.
Separately, CMS seeks feedback on its strategies to improve measurement of disparities in health care outcomes. In this RFI, the agency requests input on its framework to collect, stratify and report quality performance data across CMS programs as well as specific methods the agency could deploy within the SNF QRP specifically. The latter might include quality measures assessing a facility’s commitment to addressing health equity by taking on certain practices.
SNF VALUE-BASED PURCHASING (VBP) PROGRAM
CMS makes several proposed updates to the SNF VBP program, including policies for COVID-19-affected performance data as well as new measures and scoring methodologies for future years of the program.
Proposed Measure Suppression for FY 2023
CMS proposes to again suppress the use of data evaluating performance on the single quality measure currently used in the SNF VBP program, Skilled Nursing Facility 30-Day All-Cause Readmissions Measure (SNFRM). As in the FY 2022 SNF PPS rule, the agency remains concerned about the decrease in admissions to SNFs, regional differences in the prevalence of COVID-19, and changes in hospitalization patterns, all of which impact CMS’ ability to use the SNFRM to calculate payments for the FY 2023 program year. Under this proposal, CMS would assign all participating SNFs a uniform performance score of zero for the FY 2023 program year, resulting in all SNFs receiving an identical performance score and incentive payment adjustment.
Proposed Measure Additions
As authorized under the Consolidated Appropriations Act of 2021, the Department of Health and Human Services Secretary may add up to nine new measures in the SNF VBP program. As such, CMS proposes to adopt two new quality measures for the SNF VBP program beginning with the FY 2026 program year: Skilled Nursing Facility Healthcare Associated Infections Requiring Hospitalizations and Total Nursing Hours per Resident Day Staffing. CMS also proposes to adopt an additional measure, Discharge to Community, beginning with the FY 2027 program year.
CMS proposes to update its scoring methodology to account for these new measures beginning in FY 2026. Specifically, SNFs would be able to earn a maximum of 10 points on each measure for “achievement” (that is, performance relative to a benchmark) and up to 9 points for “improvement” (performance relative to past performance). The agency also would apply a normalization policy to translate performance scores on multiple measures into a score out of 100 total points.
Request for Comment
CMS requests stakeholder feedback on topics related to the expansion of the SNF VBP program. These topics include additional quality measures, such as a staffing turnover measure and a measure assessing COVID-19 vaccination coverage among health care personnel; updating the process used to translate performance scores into incentive payments; and validation of new measures and assessment data.
RFI: REVISING REQUIREMENTS FOR LONG-TERM CARE FACILITIES TO ESTABLISH MANDATORY MINIMUM STAFFING LEVELS
As part of the Biden-Harris Administration’s recent announcement regarding its work to improve the quality of U.S. nursing homes, CMS uses this rule to announce its intent to propose minimum standards for staffing adequacy that nursing homes would be required to meet. While the agency does not make any proposals in this rule, it does note that it will conduct a new research study to help inform policy decisions related to the level and type of staffing needed to ensure safe and quality care and expects to issue proposed rules within one year.
CMS describes the current regulatory requirements for staffing as well as prior studies on the association between staffing and health outcomes. The agency also shows trends in resident composition and care needs in long-term care facilities and outlines several considerations and approaches to address staffing concerns, including the impact of COVID-19 on the nursing home workforce. Finally, CMS requests stakeholder input to inform its policy decisions, including on evidence related to effective thresholds and cost to implement as well as experience with state-level staffing requirements.
FURTHER QUESTIONS
CMS will accept comments on the SNF proposed rule through June 10. SNF members will receive an invitation for a call to discuss the rule and inform AHA’s comments. Please contact Rochelle Archuleta, AHA director of policy, at rarchuleta@aha.org with any questions related to payment, and Caitlin Gillooley, AHA director of policy, at cgillooley@aha.org, regarding any quality-related questions.