TrendWatch: The Impacts of the COVID-19 Pandemic on Behavioral Health
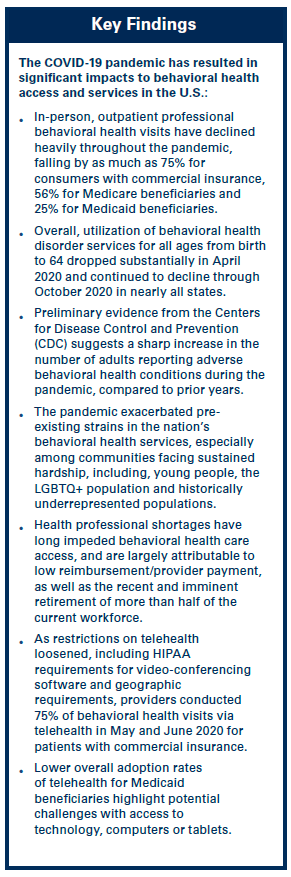 As America confronts a health care landscape deeply – and likely permanently – altered by the COVID-19 pandemic, behavioral health care access has emerged as both a challenge and opportunity. The pandemic exacerbated the need for behavioral health services while individuals with existing disorders faced additional barriers to care. However, the pandemic also inspired innovation, including escalated tele-behavioral health services and other digital solutions. There are many current topics of interest in behavioral health care, and this report focuses on COVID-19’s impact on behavioral health.
As America confronts a health care landscape deeply – and likely permanently – altered by the COVID-19 pandemic, behavioral health care access has emerged as both a challenge and opportunity. The pandemic exacerbated the need for behavioral health services while individuals with existing disorders faced additional barriers to care. However, the pandemic also inspired innovation, including escalated tele-behavioral health services and other digital solutions. There are many current topics of interest in behavioral health care, and this report focuses on COVID-19’s impact on behavioral health.
Definition: Behavioral Health Disorders and Services
In the Notice of Benefit and Payment Parameters for 2023 CMS finalized:
In this report, we define behavioral health disorders as both mental illness and substance use disorders. Mental illnesses are specific, diagnosable disorders characterized by intense alterations of thought, mood and/or behavior. Substance use disorders involve the recurrent use of alcohol and/or drugs, including medications, which cause clinically significant impairment. Persons with behavioral health care needs may experience one or both conditions, as well as physical co-morbidities.
In 2019, the American Hospital Association (AHA) published a TrendWatch report and Market Insights Report that provided background on behavioral health care access, utilization and payment. This report builds on that foundation to describe COVID- 19’s impact on behavioral health care.

Even before the COVID-19 public health emergency, the demand for behavioral health services was on the rise. An estimated 52 million adults in 2019, or approximately 21% of the U.S. adult population, reported having mental, behavioral or emotional disorders. Additionally, 20 million people aged 12 or older attested to having substance use disorders, which are characterized by alcohol abuse, illicit drug abuse, or both.
Patients exhibit behavioral health care needs in almost every care setting, including emergency departments and acute inpatient units such as oncology, cardiology and orthopedics, as well as in specialized psychiatric and behavioral health units such as substance use disorder, geriatric, eating disorder and medical/ psychiatric disorder units. According to a 2015 report from the Agency for Healthcare Research and Quality, one of every four patients admitted to a general hospital is diagnosed with a behavioral health disorder.
This prevalence of behavioral health issues and their interactions with – and impact on – physical health pressures caregivers. This demand is exacerbated by an ongoing national shortage of behavioral health providers, due in part to inadequate reimbursement rates. For example, Medicaid is the single largest payer for behavioral health services, with nearly a quarter of adult Medicaid and Children’s Health Insurance Program (CHIP) beneficiaries receiving mental health or substance use disorder services. The Medicaid program also reimburses at the lowest rates of any payer., Patients sometimes decline or delay treatment due to lack of insurance coverage and/or high out-of-pocket costs. The inadequate enforcement of mental health parity laws, high prescription costs and shortages of in-network providers all contribute to these high costs.
View the detailed Trendwatch below.


