Health Care Leaders Brace for Pandemic’s Resurgence
Signs of a potential COVID-19 resurgence are all around us. Daily case counts pushed beyond 60,000 as of Oct. 21. Hospitalizations due to the virus are rising in many regions of the country, with the Mountain West and Midwest breaking records. And, in a chilling reminder of the early days of the pandemic, several states are planning again to set up field hospitals.
 All of this has left health care leaders with one eye focused on recovery and financial viability and the other on the resiliency of front-line caregivers, many of whom have lasting effects from what they experienced during the initial waves of COVID-19.
All of this has left health care leaders with one eye focused on recovery and financial viability and the other on the resiliency of front-line caregivers, many of whom have lasting effects from what they experienced during the initial waves of COVID-19.
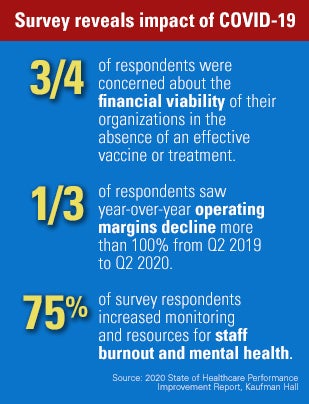
The new reality is that any hope of COVID-19 subsiding soon are fading fast. In fact, new survey data from Kaufman Hall on the state of health care improvement from the impacts of COVID-19 found that nearly three-fourths of respondents were concerned about the financial viability of their organizations in the absence of an effective vaccine or treatment.
In follow-up interviews with seven of the responding health care organizations, respondents to the survey were unanimous in that they don’t expect a return to anything resembling pre-pandemic norms until 2022. Moreover, one-third of respondents saw year-over-year operating margins decline more than 100% from Q2 2019 to Q2 2020. Volumes are recovering slowly in most service areas, with only one service area — oncology — returning to more than 90% of pre-pandemic levels, most respondents said.
Resolving financial challenges brought on by the pandemic will take time, but a more immediate concern for many organizations will be ensuring the resilience of their front-line caregivers. Survey data showed that 75% of respondents increased monitoring and resources for staff burnout and mental health.
Tending to the mental health needs of the public also will be a priority. As of July, the Centers for Disease Control and Prevention estimates that 41% of people have experienced symptoms of an anxiety or depressive disorder as a result of the pandemic, notes Brett Hart, chief behavioral health officer for Centene Corp., the nation’s largest Medicaid managed care organization. A medical study from June reported a 47% rise in calls to national crisis hotlines, Hart writes in a recent Modern Healthcare article.
Add to these concerns the fact that supply costs continue to rise and personal protective equipment shortages still exist, and it’s easy to envision a challenging fall and winter for hospitals and health systems.
 The good news, as the Kaufman Hall research points out, is that many provider organizations have greatly improved their agility and resilience in adapting to rapid change during the pandemic. Many have also reaped dividends from their pre-pandemic investments in data analytics to improve decision-making during the crisis. In addition, providers have greatly strengthened their relationships with other health systems to better coordinate response, and improved communication with local and state governments, schools and community organizations. Likewise, with providers nationally demonstrating early on in the pandemic the ability to rapidly scale telehealth services, this serves the field well in the event of a resurgence. The Kaufman Hall survey found that 56% of respondents saw more than 100% growth in the number of telehealth visits their organizations provided.
The good news, as the Kaufman Hall research points out, is that many provider organizations have greatly improved their agility and resilience in adapting to rapid change during the pandemic. Many have also reaped dividends from their pre-pandemic investments in data analytics to improve decision-making during the crisis. In addition, providers have greatly strengthened their relationships with other health systems to better coordinate response, and improved communication with local and state governments, schools and community organizations. Likewise, with providers nationally demonstrating early on in the pandemic the ability to rapidly scale telehealth services, this serves the field well in the event of a resurgence. The Kaufman Hall survey found that 56% of respondents saw more than 100% growth in the number of telehealth visits their organizations provided.
A new report from the AHA, “Responding to COVID-19,” also can help hospitals and health systems prepare for and respond to a resurgence of the pandemic. It provides a compendium of select AHA tools and resources to assist health care leaders in responding to the virus, including:
- Recovery, the return of elective care and capacity planning.
- Protecting and enabling health care workers.
- Caring for patients and communities.
- Addressing health care disparities.
- Telehealth and virtual care.
- Cybersecurity resources.



